Epileptic Disorders
MENUThe 2017 ILAE classification of seizure types and the epilepsies: what do people with epilepsy and their caregivers need to know? Volume 20, issue 2, April 2018
“If names be not correct, language is not in accordance with the truth of things. If language be not in accordance with the truth of things, affairs cannot be carried on to success” (Confucius, Analects, 6th century BC).
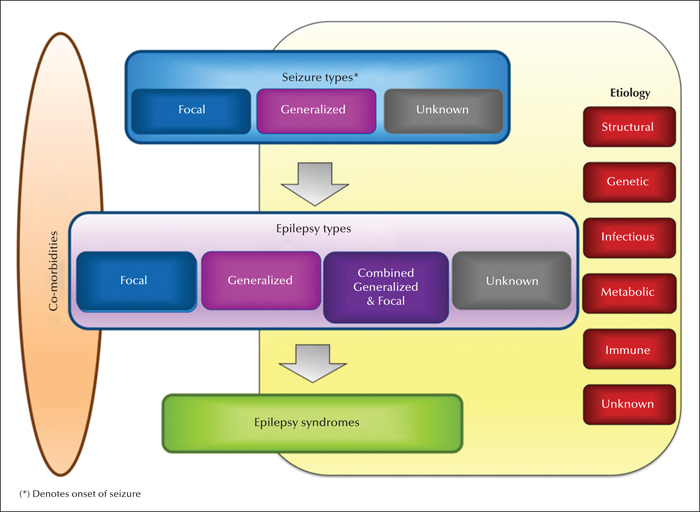
In 2017, the International League against Epilepsy (ILAE) published in two articles an updated classification of seizures and the epilepsies, together with an instructional manual on how to apply the seizure classification (Fisher et al., 2017a, 2017b; Scheffer et al., 2017). These were the first new official papers on classification from the ILAE since 1989. The new framework is illustrated in figure 1. The first two papers highlight changes in the revised classification (Fisher et al., 2017a; Scheffer et al., 2017), while the third provides guidance on how best to use the updated seizure classification terminology in everyday clinical practice (Fisher et al., 2017b). One of the main reasons to revise the epilepsy classification was to use more accessible, transparent language suitable for clinicians, scientists, and patients. The aim of this companion piece is to present these new concepts to other non-specialist professionals and to people with epilepsy and those who care for them. Everyone now has access to medical information via the internet which was not available to previous generations, and so it is increasingly important that medical concepts are as clear and unambiguous as possible. This paper may also help doctors to explain epilepsy to affected individuals and their families.
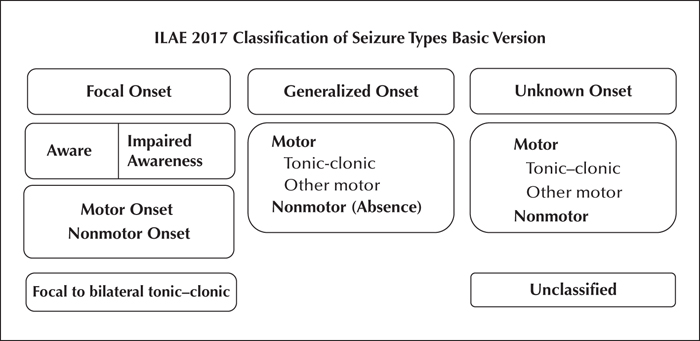
Each of the three publications will be discussed separately. We have not attempted to combine them, since this would have added to the risk of inadvertently including misinterpretations. There is substantial overlap among them and so some repetition is inevitable. The basic and operational classifications of seizure types are shown in figures 2 and 3. A revised glossary of terms is also included (table 1). This paper follows the formats of the three new publications and attempts to provide an interpretation of the content. The reader may find it helpful to consult the original papers (which can be freely downloaded from https://www.ilae.org/guidelines/definition-and-classification) to obtain a more complete picture of the often-complex concepts under discussion.
Paper 1: ILAE classification of the epilepsies (Scheffer et al., 2017)
This paper presents a new framework for classification of the epilepsies with three levels, as well as a major focus on looking for a cause and identifying any associated disorders, or co-morbidities, at all stages along the diagnostic process. It begins with seizure type(s) defined by their type of onset (focal; generalized; unknown), then epilepsy type and thirdly, epilepsy syndrome. Wherever possible, the aim is to classify a patient's epilepsy in a way that is recognisable across a range of individuals experiencing the same pattern of seizures, age at onset, and electroencephalographic (Koutroumanidis et al., 2017a, b) and imaging features, who often share a similar cause for their epilepsy. When possible, this may allow diagnosis of a specific epilepsy syndrome to be attached to the collection of symptoms and signs. In some cases, only the epilepsy type will be diagnosable, and no syndrome name will apply.
The revised classification also emphasizes the importance of considering the cause, or aetiology, of the patient's epilepsy from the initial consultation onwards. It presents six broad headings for the aetiologies (figure 1). Attached to this framework is also a section for comorbidities, which are conditions associated with epilepsy. These include issues such as learning problems, intellectual disability, and psychiatric features such as depression, psychosis, and autism spectrum disorders; comorbidities will not be discussed in detail in this paper.
This new classification provides a better understanding of the types of seizures that the person suffers from and the likely cause and probable long-term outcome of the epilepsy. Correct classification can also help with the choice of drug treatment and point to the possibility of epilepsy surgery, if optimal seizure control is not obtained with medication. This process ideally requires access to specific investigations, such as a video-EEG (for a detailed educational publication on EEG characteristics see Koutroumanidis et al., 2017a, 2017b) and brain imaging, together with a range of blood studies, including genetic and/or metabolic screening when indicated, aimed at identifying the cause of the epilepsy. The current proposals are based on the latest scientific information, which has been reviewed by experts in epilepsy from around the world.
Classification of the epilepsies
This revised classification attempts to cover the development of epilepsy across a range of global environments. It assumes that the clinician has already made a definite diagnosis of an epileptic seizure and is not meant to be a diagnostic algorithm to distinguish epileptic from nonepileptic events. Where possible, the diagnosis should take into consideration the seizure type or types, epilepsy type, and epilepsy syndrome, as well as the specific cause underlying the problem (figure 1).
Seizures can be divided into those with focal onset, generalised onset, and unknown onset. Some focal seizures can spread quickly to produce a tonic-clonic seizure, previously known as a “grand mal” seizure or convulsion. The epilepsy types can be focal, generalized or both. In some circumstances, this will be unclear (“unknown”). Many syndromes include more than one type of seizure.
Generalized seizures
In these events, the abnormal electrical activity (as judged by behaviour or EEG) apparently originates simultaneously on both sides of the brain and spreads rapidly via neuronal networks. Most people will recognise a generalized tonic-clonic seizure (convulsive seizure) as a typical sign of epilepsy. However, there is a range of other generalized seizures. These include absences, where the affected individual, usually a child or adolescent, loses awareness for a number of seconds resulting in a blank stare. This may be accompanied by more subtle signs, such as flickering of the eyelids and mouth movements. Myoclonic jerks are also types of generalized seizures and occur when there is a sudden rapid contraction of a group of muscles. They can affect the head, arms, legs or whole body and can be unilateral or bilateral. The affected person may drop or spill things and, if the jerking is severe or occurs in a young child, they can fall. Because the jerk can last less than a second, there is no obvious loss of consciousness. Frequent myoclonic seizures can also occur in some severe epilepsies of infancy and early childhood. Other less common generalized seizure types include atonic (loss of muscle tone) and tonic (more prolonged increase in muscle contractions) seizures, both of which can also result in falls or drop attacks and epileptic spasms.
Focal seizures
In these events, the abnormal electrical activity originates on one side of the brain, although in some situations it can spread to the other side later in the seizure. Focal seizures can present with a range of symptoms, depending on the site of origin of the abnormal electrical discharges and the extent and speed of their spread in the brain. Awareness may be present, reduced or absent. Sometimes, there is jerking of one arm and/or leg. Epileptic spasms can also have a focal origin. The abnormal electrical activity can move quickly from a focal seizure to a tonic-clonic seizure, affecting both sides (bilateral), known as a focal to bilateral tonic-clonic seizure. The EEG may suggest an area in the brain from where the seizure is arising, and brain imaging may demonstrate a structural cause for the seizures, such as scarring, a developmental anatomical abnormality (brain malformation), an abscess, stroke or tumour. In around a third of people with focal seizures, brain imaging will be reported as normal.
Focal and generalized seizures
The next group consists of people who have both focal and generalized seizures. The VEEG (Koutroumanidis et al., 2017b) can be helpful in defining this category. In the severe epilepsies of infancy and childhood, the EEG is often markedly abnormal. There is often evidence of more than one type of seizure.
Unknown
Occasionally, the doctor cannot be certain whether the epilepsy is focal or generalized. This is more common where there is limited access to VEEG studies and modern brain imaging such as magnetic resonance imaging (MRI).
Epilepsy syndromes
The third level of diagnosis, wherever possible, is the identification of an epilepsy syndrome. This includes a cluster of features, including seizure types, EEG changes, brain imaging abnormalities, and genetic analyses that add up to a recognisable pattern. Different syndromes can occur at different ages in life, and an accurate diagnosis often provides useful information on the likely outcome. Some syndromes are associated with other symptoms, such as intellectual and psychiatric problems, which may play an important part in the overall clinical picture. The recognition of a syndrome can help to determine the cause, treatment, and outcome of the epilepsy. The educational ILAE website (www.epilepsydiagnosis.org) and the website of the ILAE educational journal Epileptic Disorders (www.epilepticdisorders.com) provide descriptions, EEGs, and video examples of many seizure types and epilepsy syndromes. New epilepsy syndromes are described in the emerging literature fairly often, and there is currently no “official” ILAE list of all the syndromes. All this information is readily available to people with epilepsy and their families.
Among the generalized epilepsies are a well-recognised group of common epilepsy syndromes: childhood absence epilepsy, juvenile absence epilepsy, juvenile myoclonic epilepsy, and generalized tonic-clonic seizures alone. They have previously been known collectively as the “idiopathic generalized epilepsies”, which means that the exact cause is unknown, but the evidence is strongly in favour of a genetic basis. Less frequently, they may have an obvious hereditary component, i.e. run in families. In the new classification, they can be called “genetic generalised epilepsies” or “idiopathic generalised epilepsies” depending on whether the clinician finds the term “genetic” acceptable for their patient and family.
Another group of focal epilepsy syndromes that occur in childhood have a self-limited course. Often the diagnosis is made by the presence of spikes in a particular pattern on the EEG that relate to electrical malfunctioning in a particular part of the brain (Koutroumanidis et al., 2017a). These conditions may be treatment responsive and self-limiting, and usually affect the temporal, frontal or occipital lobes in the brain. Recognition of a particular syndrome can provide important information on the best approach to management and can shine a light on the likely long-term outcome.
Causes of epilepsy
As soon as a person has their first epileptic seizure, everyone involved wants to know the cause. A range of possibilities can be recognised, which may help with understanding the problem and point to its optimal treatment. It should be appreciated that a specific reason why seizures occur cannot always be identified. As our knowledge improves and the availability of more sophisticated investigations is becoming more widespread, this “unknown” group of epilepsies is becoming smaller. The six recognised causative categories under this heading are highlighted in figure 1. It should be appreciated that the patient's epilepsy may belong to more than one group of causes. For example, a genetic disorder may cause a structural abnormality of brain development, which leads to the epilepsy. This would be termed a “structural” and “genetic” cause.
Structural causes
Structural causes of epilepsy can be recognised via a range of brain imaging investigations. The anatomical abnormality needs to relate directly to the symptoms and signs of the seizures, since many people without epilepsy have abnormal brain imaging. The past history may be a useful contributory factor, e.g. a previous head injury, stroke, tumour, birth injury, brain infection, etc., which may be associated with the particular type of seizures under scrutiny. This association may take some time to establish. In some cases, a positive brain scan will provide the basis for subsequent epilepsy surgery, usually after treatment with appropriate antiepileptic drugs has failed. Structural abnormalities are usually acquired, although on occasion the patient may be born with an anatomical defect that may be part of a genetic syndrome. Recognising the cause of the epilepsy can be reassuring to all concerned and can point the way to the best avenue of care. The more advanced the available technology, the more likely will a relevant anatomical abnormality be identified.
Genetic causes
Genetics can be considered as the part of biological sciences that is concerned with the study of genetic variation and heredity. Genetic factors are probably the most important single causative group for the epilepsies. However, we still cannot find a precise defect in most people with suspected genetic epilepsy. Epilepsies can be called “genetic” if we know that there is a strong family history, whether an implicated gene is discovered in the family or not. We know that some common types of epilepsy are largely caused by genetic factors. For instance, when epilepsy develops in identical twins, both twins will almost always be affected. Several hundred genes have now been linked to different epilepsies. The vast majority of these are associated with rare syndromes, which most often present in early childhood. Information in this area is expanding with the development of more sophisticated methodology. Identification of a potential genetic cause for the epilepsy can provide insights into what medication to choose and sometimes what not to choose for treating the seizures. Occasionally, an underlying genetic cause cannot be identified, despite the fact that a number of people in the family have a similar type of epilepsy. In addition, a range of different types of seizures can occur in some families.
Although genetic syndromes are most often diagnosed in infancy or childhood, genetic disorders can also arise in adolescence or even later in adult life. Sometimes, a single gene defect is the culprit, while in other cases, multiple genes are involved in causing the individual's epilepsy. Interestingly, the same genetic abnormality can produce different types of seizures in different people, and different gene defects can cause the same epilepsy syndrome. The same genetic abnormality can result in both mild and severe epilepsies. There must, therefore, be other factors that influence how the implicated gene affects the individual, e.g. interacts with other genes. Often, it is thought that multiple genes contribute to the clinical picture, especially in the common situation where there is no family history of epilepsy.
It is important to appreciate that a genetic cause does not necessarily mean the person has an inherited epilepsy. An affected individual can have a new gene abnormality, or mutation, that does not occur in anyone else in the family. However, this person may have a risk of subsequently passing on the abnormal gene to his or her children. To make matters even more complicated, although around 50% of the children may inherit the mutation, this does not necessarily mean that they will all develop epilepsy, as this can depend on the presence of a range of other, as yet, unidentified factors. The next decade or two will see an acceleration in our understanding of the genetic bases of the epilepsies.
Infectious causes
Any infection in the brain or its lining, whether acute or chronic, can produce seizures. Much depends on the part of the world where the infection is contracted in terms of the likely culprit. The commonest infective cause of epilepsy is neurocysticercosis, a tapeworm that is found commonly in Latin America, Africa and Asia. The epilepsy is caused by ingestion of tapeworm eggs. These hatch in the stomach or intestines and the worms migrate to the brain, producing characteristic cysts. Other potential infective causes include HIV, tuberculosis, malaria, bacterial meningitis, and viral encephalitis. Treatment of the infection is an essential component of the therapeutic strategy. The more widespread the brain damage, the more likely the seizures will be difficult to control. Sometimes, there is only a history of a previous infection in infancy or childhood, which is assumed to be the cause of epilepsy later in life.
Metabolic causes
There are a number of unusual and complicated disorders involving the production or breakdown of natural substances in body cells that are also associated with the development of epilepsy. The biochemical changes produced can result in seizures as part of the symptoms of the condition. Thus, they may only make up a small part of a more complex clinical picture. Many of these conditions have a genetic basis. Recognition of these rare disorders is essential to lead the clinician down the correct treatment path, as in certain cases replacing a missing chemical compound or vitamin may be indicated rather than, or in addition to, providing standard antiepileptic drug therapy.
Immune causes
Among the wide range of disorders that can be associated with the production of seizures are immune conditions, where the body attacks its own tissues by the production of antibodies. The epilepsy can be a consequence of inflammation in the brain and management may require specific medication to damp down the immune system, i.e. treat the cause of the seizures rather that the seizures themselves. These autoimmune-mediated epilepsies are unusual conditions that must be recognised promptly to ensure optimal management.
Unknown causes
Some epilepsies do not have a recognisable cause. Much depends on the availability of routine, and sometimes more sophisticated, investigations. Thus, the number of people who have epilepsy for no obvious reason is higher in resource-poor countries. This often brings its own problems, since all affected individuals and their families want to know why they have developed seizures and why their treatment may be lifelong. The situation may be even more stressful for the family of an affected infant or child in the developing world.
In summary, It is hoped that this updated “Classification of the epilepsies” will help to improve the diagnosis, focus better on the cause, and provide a useful guide to management in as wide a range of people with epilepsy as possible. Thus, we can all understand what is happening in the affected person's brain and what is the best course of action to treat the disorder. This new classification is also an important clinical tool for communication among people with epilepsy and their doctors.
Paper 2: Operational classification of seizure types by the International League Against Epilepsy (Fisher et al., 2017a)
This paper presents a revised classification of seizure types, which depends on how seizures present to people with epilepsy and their families, carers, and doctors. These terms are largely based on what is observed during the episodes. The aim is to provide a common language so that everyone involved knows exactly what is meant by each type of seizure. Previous terms that were unclear to non-specialists and people with epilepsy have been largely abandoned. This new approach does not represent a major change but makes recognising seizure types more straightforward. The major categories include focal onset and generalized onset seizures, and also take cognisance of situations where the onset of the seizure is unknown. Some seizures involve movement of particular parts of the body and others affect awareness. These can both be types of focal seizures and the presentation depends on where the abnormal electrical activity arises in the brain and how far and how fast it spreads. Seizures usually involve a network of changes and are not just symptoms of a local problem.
Methods of classification of epileptic seizures
Seizures can be defined as “transient symptoms and/or signs due to abnormal and simultaneous neuronal activity of a population of neuronal cells in the brain”. The first goal of the doctor is to ensure that the episodes are definitely epileptic seizures. The next step is classifying the seizure type, based on its onset characteristics. This provides a useful group of clinical characterisations that can be used for communication among people with epilepsy, their families, and their doctors. Using this agreed terminology can also help with teaching and research, since everyone should be speaking the same language. Correct classification of the epilepsy is important too for insurance policies, regulatory agencies, advocacy groups, and medical reports.
Seizure classification
Figure 2 shows the basic updated seizure classification, whereas figure 3 presents an expanded version that covers the most common or most important types of seizures in greater detail, although not every seizure type can be represented in a classification, and in clinical practice a detailed description of the symptoms observed remains essential. All terms that are likely to be employed by specialist neurologists, paediatricians or psychiatrists have been included in this latter description. Some relevant terminology is explained in the attached glossary (table 1). Focal onset seizures may be accompanied by continued awareness, depending on the site of onset and extent and speed of the spread of the abnormal electrical activity. Often, however, the individual will lose awareness at some stage during the focal seizure, which is now referred to as a “focal impaired awareness” seizure. Arrest of movement or loss of memory for events occurring during the seizure can also be part of the seizure pattern. People with atonic or myoclonic seizures and epileptic spasms will usually retain awareness, or loss of awareness will be so brief as to be hard to detect. Cognitive seizures refer to problems during the seizure such as impaired speech, hallucinations, illusions, or feelings of déjà-vu. Emotional seizures can manifest as anxiety, fear, joy or any other emotion. An absence is atypical when it differs from the usual fast onset and EEG pattern of a 3-4 per second generalized spike-wave pattern. If seizure patterns are not clearly recognisable, the episodes will remain unclassified.
Structure
The columns in the classification allow specific seizure descriptions to be included under the general headings of focal, generalized or unknown onset (figures 2, 3). Awareness is an optional extra in the focal seizure column, but it is so important in influencing the impact of a seizure that it has been given special mention. We employ an operational definition of awareness as knowledge of self and environment. In this context, awareness refers to perception or knowledge of events occurring during a seizure, not to knowledge of whether a seizure has occurred. Level of awareness may vary among similar seizures in the same individual. Sometimes, loss of awareness is not complete or always recognised by the person experiencing the seizure and by bystanders. Abnormal movements may be present. The first prominent sign usually determines the seizure classification, because the first manifestation marks the part of brain where the seizure originates. More prominent features may ensue and be worthy of mention, but the first sign or symptom classifies a focal onset seizure. The exception to this rule is awareness, such that a seizure is a focal impaired awareness seizure if awareness is impaired at any time during the seizure. The beginning of the seizure is, therefore, important in helping with its classification. The greater the observed detail of each episode, the more likely will the seizure classification be correct.
Seizure activity progresses through brain networks and can arise from different anatomical sources. The abnormal electrical activity spreads, bringing with it a variety of symptoms and signs. Some people will have more than one type of seizure. Generalized seizures can be divided into motor and absence seizures. Other types include myoclonic, atonic, tonic or a combination that can allow a specific pattern to be recognised, leading to the diagnosis of an epilepsy syndrome. Seizures of unknown origin can be regarded as “unclassified” with or without other features, such as motor, nocturnal, tonic-clonic, epileptic spasms (which can be called “infantile spasms” in children less than a year of age), and behavioural arrest. These additional terms allow better description of the episodes and can be useful to the doctor in narrowing down the epilepsy type, with implications for causation and treatment.
There is an overlap between focal and generalized seizures, since both have to start somewhere, and it may not be possible with limited investigational tools to be certain exactly what is happening in the brain at the onset of the abnormal electrical activity. The episode may only be recognised when it is already affecting both sides of the brain. In some instances, the exact sequence of events can only be determined by careful study of a video-EEG, which is unusual even in countries with the most sophisticated healthcare systems. Focal onset can often, however, be obvious with an aura of déjà-vu, a strange taste or smell, or a rising sensation in the stomach, followed by loss of awareness, lip-smacking, and hand rubbing. The term “aura” has been retained since, if presenting alone, is a focal aware seizure. Unwitnessed seizures or those occurring during sleep are common. If they are infrequent, it may not be possible to be certain of the seizure type, or even to discern whether the episode has a focal or generalized onset. Thus, “unknown onset” can be regarded as an acceptable description in some instances until more useful information becomes available. “Unclassified” should be regarded as a term of last resort, where the clinician is confident that the events represent epileptic seizures, but cannot further classify them.
Whether a person retains or loses consciousness during a seizure can be a complicated issue. This can matter greatly since episodes accompanied by impaired consciousness are often considered differently, e.g. with respect to driving, impaired learning capacity, and poor memory and recall. Consciousness, therefore, is an important concept in classifying focal seizures. However, different levels of impairment of consciousness can occur in the same person and it can be difficult to be certain that some seizures are not associated with some reduction in awareness or memory. The affected individual may not be certain whether full consciousness is retained during every episode. A person may be conscious during the seizure, but not necessarily fully aware of everything going on around them i.e. unaware is not the same as unconscious. One approach is to define the episode as a focal aware or focal impaired awareness seizure. From a practical perspective, the affected individual should be able to recall and relate all aspects of the event, even if unable to respond during the seizure; otherwise, impaired awareness must be assumed. Responsiveness, awareness, and consciousness are not usually present during generalized seizures, so these features are not used to classify generalized seizures.
Knowledge of the cause of the epilepsy can greatly help with seizure classification. Thus, evidence of an anatomical abnormality in the brain, which matches the symptoms and signs of the seizures, usually supports their focal onset. With improved brain imaging, this scenario is being increasingly recognised in everyday clinical practice. A clear history from the affected person, accompanied by an eyewitness to the attack, provides the most useful diagnostic information. Videos from a smart phone brought to the clinic by the family, EEG patterns, brain imaging, and laboratory tests, including those for antibodies or gene mutations, can also help to confirm the seizure classification and aid in making an epilepsy syndrome diagnosis. Supportive information, however, may be less available in resource-poor countries, although this should not prevent the neurologist from trying to identify the correct seizure type and attempting to make the diagnosis of an epilepsy syndrome.
A number of terms have been discarded in this new classification, including “simple partial seizure”, “complex partial seizure,” “psychic seizure,” and “dyscognitive seizure.” Reorganisation of some seizure types has taken place to keep up with new knowledge. Terms like “epileptic (infantile) spasms”, “tonic-clonic”, “atonic” and “myoclonic seizures” can now appear under the headings of seizures of focal, generalized and unknown onset. A number of new seizure descriptions have been included, such as automatism, cognitive, emotional, hyperkinetic, and behavioural arrest. A few unusual seizure types are now regarded as generalized, such as absence seizures with eyelid myoclonia and myoclonic absences. Thus, certain seizure types now appear in multiple categories. The new approach provides a detailed descriptive template for seizures.
Paper 3: Instruction manual for the ILAE 2017 operational classification of seizure types (Fisher et al., 2017b)
This third article contains substantial overlap with the other two papers. The goal here is to provide guidance on how best to use the new classification of seizure types. A glossary of terms has been included, which has been amended in this paper to make the terminology more accessible to people with epilepsy and their families (table 1). Key symptoms and signs provide the basis for the classification of the seizures. Focal seizures can progress to bilateral tonic-clonic episodes. Generalized seizures involve both sides of the brain from the outset. As discussed previously, focal onset seizures can be further designated according to whether awareness is retained or impaired. Seizures with a motor onset may have other features, which can be described as atonic, automatism, clonic, epileptic spasms or have hyperkinetic, myoclonic or tonic activity. Non-motor seizures can display a range of elements including autonomic, behavioural, cognitive, emotional, and sensory dysfunction. The earliest symptoms or signs usually define the seizure type. Generalized motor seizures can be characterised as atonic, clonic, epileptic spasm, myoclonic, myoclonic-atonic, myoclonic-tonic-clonic, tonic, and tonic-clonic. Non-motor seizures are typical or atypical absences or seizures that present myoclonic activity or eyelid myoclonia. Seizures of unknown onset can have components that are classified as motor, non-motor, tonic-clonic, epileptic spasm, or behavioural arrest.
Seizure classification can be followed by a description of other features of the seizure. Although such a description does not change the seizure type, it may be very helpful in portraying the manifestations of a seizure. The more detail included in the description, the more likely can a cause be inferred or identified, and a specific syndrome recognised. A range of old-fashioned terms has been discarded in favour of a more descriptive approach. This paper also provides a “user manual” for the new classification aimed at encouraging the adoption of the new system by all doctors and the wider community of health professionals. People with epilepsy are also required to understand and adopt this modified language, although perhaps not in too much detail.
Application
An accurate classification of seizure types requires careful observation of the episodes with a degree of consistency that supports the appropriate terminology. This relies on a good history and a witnessed description. A home video of the episodes can provide invaluable information. There is some overlap regarding the different types of seizures. Taking time to get things right is essential, since the likely cause and the most effective treatment can vary. Outcomes too can be different, depending on the seizure and syndrome classification. An understanding of the sequence of events may contribute to their correct interpretation. As discussed throughout this paper, EEG and brain imaging are often essential to help the doctor reach the correct conclusion regarding the type of epilepsy and its cause. One of the major problems is our lack of understanding of the processes that underlie the production of different types of seizures and so we are usually treating the symptoms and not the cause of the problem. Nevertheless, if we are to eventually understand these processes, we will all need to speak the same language, e.g. identify correctly the seizure types and epilepsy syndromes, wherever the affected person comes from around the world.
We have included in this discussion paper both the basic and extended versions of the classification in figures 2 and 3 (Fisher et al., 2017a). Focal onset seizures start in a particular part of the brain and generalized seizures are usually bilateral at onset. In some circumstances, the site of origin of the episodes cannot be accurately identified. On other occasions, the classification may be unclear, particularly if sophisticated modern investigations are not available. Helpful information can include lack of awareness, symptoms or signs affecting a particular part of the body, responsiveness during an episode, and progression of the seizure in a consistent pattern. Sometimes, coordinated motor activity can occur, which can be complicated, e.g. walking in circles. The affected person is usually unaware of what is happening around them. This is known as “automatism”, meaning semi-automatic movements. Absence seizures can present, usually in children or teenagers, with sudden cessation of activity, accompanied by loss of awareness. An EEG is often essential to make a correct diagnosis (Koutroumanidis et al., 2017a, 2017b). Seizures of uncertain onset can be motor, non-motor or unclassified. Some description of the episodes is better than none, even if it is incomplete.
The expanded classification provides a more detailed breakdown of the seizure types, and is particularly useful for neurologists and will be critical for research purposes. This detailed approach will have even greater interest for epilepsy specialists and may not be as relevant to paediatricians or general practitioners. The wide range of descriptions allows a clearer understanding of the seizures, which is of particular importance for some of the complex epilepsies in infants and young children. Again, the presence or absence of awareness, motor signs, and a good description of the episodes can provide a more accurate picture of what is happening in the brain. This information may have little discriminatory value to the person with epilepsy and their family, but can be very helpful to their doctor in understanding better the underlying disorder and choosing the most appropriate approach to treatment.
The terminology used in these three papers will be of value in explaining what is happening before, during, and after a seizure, and so should be accessible to everyone involved in epilepsy care. How much of this should be discussed with the affected person and their family depends on the specific requirements of all concerned. These descriptive terms are more scientifically meaningful than the previous discarded terminology, such as “grand mal” and “petit mal”. There are many symptoms associated with seizures and these should be accurately described so that everyone is speaking the same language. This detail may be particularly valuable if epilepsy surgery is being considered. Accordingly, the content of this third contribution has less relevance to people with epilepsy and their families than the information contained in the other two papers. Nevertheless, the doctor can expect to have to respond to questions about these symptoms and signs, and will be required to explain how they relate to the seizures, their cause, their investigation, and their treatment.
Much of the information in these papers refers particularly to focal seizures. Generalized seizures are often more obvious and tend to have fewer nuances. Generalized tonic-clonic seizures, for instance, begin, progress, and end with jerking of the arms and legs on both sides of the body, together with the head, neck, face, and body on most occasions. These are descriptions about what exactly happens during the episode and can contribute to making an accurate diagnosis of a syndrome. Non-motor episodes comprise a range of different types of absence seizures. Rapid eyelid jerking with upward deviation of the eyes is a rarer type of absence seizure with eyelid myoclonia, often triggered by photic stimuli, such as bright sun. If all the necessary information is not available, a decision to call the seizure “unclassified” may be taken.
Rules for classifying seizures
The first step is to decide whether the episode can be classified as focal or generalized and then consider whether awareness is affected or not. The starting point for focal onset seizures should be identified, as well as whether the person stops doing what they were doing before the episode started. Motor and non-motor features should be carefully documented. For generalized tonic-clonic seizures, any symptoms or signs at onset should be explored to provide a clue regarding the anatomical site of origin for the episode, which can often later be confirmed by EEG and brain imaging. Specific features can be helpful in differentiating the various types of non-motor seizures, particularly in infants and young children.
Conclusions
These three papers have reworked the 1981, 1985 and 1989 classifications of seizures and epilepsy syndromes to provide a modern descriptive template (Fisher et al., 2017a, 2017b; Scheffer et al., 2017). Their content overlaps and so some repetition is inevitable. The aim of this companion piece is to make this new thinking available to people with epilepsy and those who care for them. This provides them with a description of the terminology used by their doctors so that everyone understands the types of seizures that the person suffers from and sometimes also the epilepsy syndrome. This information can influence decisions regarding investigations, treatment options, and long-term outcomes. Old-fashioned terms such as “grand mal”, “petit mal” and “simple and complex partial seizures” have been discarded. This new terminology is available on the internet and increasingly people are aware that they can explore the latest thinking on causes and treatment of any form of epilepsy for themselves. All the necessary clinical details may not be available for every affected individual and so some doubt about the classification will sometimes remain. A careful accurate description of the episodes is an essential component for the correct interpretation of the symptoms and signs. Our goal in writing this manuscript is to ensure that, wherever possible, people with epilepsy and their doctors speak the same language.
Disclosures
Martin Brodie has no conflicts of interest to disclose in relation to this paper except for his position as President of the International Bureau for Epilepsy. Sameer Zuberi has no conflict of interest to disclose in relation to this paper except for his position as Chair of the ILAE Commission for Classification and Terminology. Ingrid Scheffer has no conflict of interest to disclose in relation to this paper except for her position as former Chair of the ILAE Commission for Classification and Terminology and recent Chair of the Task Force for Classification. Robert Fisher has no conflicts of interest to disclose other than serving as Chair of the ILAE Task Force on Seizure Classification.