Epileptic Disorders
MENUIctal SPECT reveals different epileptogenic zones in frontal lobe epilepsy Volume 20, issue 5, October 2018
Functional and structural neuroimaging techniques are important in the evaluation of patients with focal epilepsies for localization of the epileptogenic zone. Ictal SPECT has a high localizing and lateralizing value in patients considered for epilepsy surgery (Duncan, 1997). Superimposition of subtraction images of interictal and ictal SPECT onto MR images (SISCOM) improves the localizing value significantly (Tan et al., 2008). However, spread of epileptic activity may lead to falsely localizing results of ictal SPECT (Noachtar et al., 1998). Therefore, early injection and simultaneous EEG are important prerequisites.
Case study
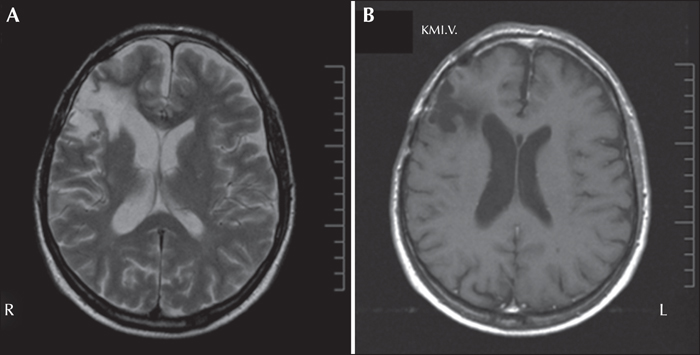
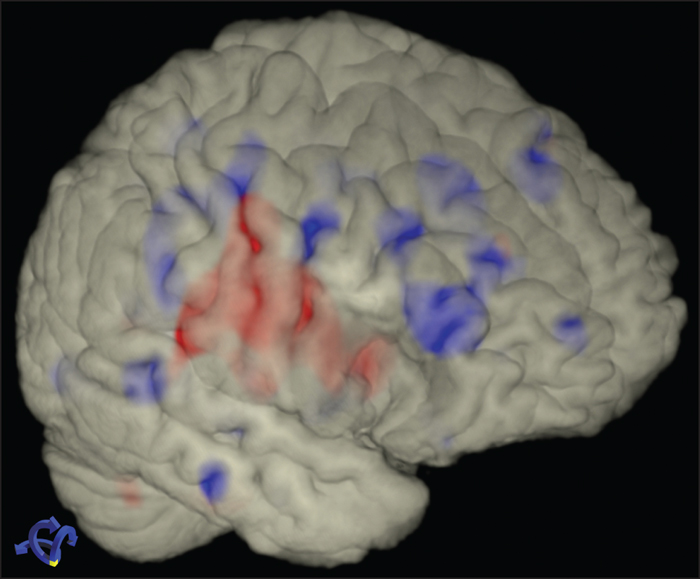
A 56-year-old male was diagnosed with a right frontal tumour after his first generalized tonic-clonic seizure. Tumour resection was performed and histology revealed an anaplastic astrocytoma WHO Grade III (figure 1). He received phenytoin for three months and remained seizure-free off medication for almost seven years. He then had a relapse with a generalized tonic-clonic seizure during night sleep. Antiepileptic treatment failed to control clonic seizures of the left face and the tongue with preserved consciousness. He was admitted to the Epilepsy Monitoring Unit of the University of Munich for continuous non-invasive video-EEG monitoring. A 40-channel video-EEG evaluation with scalp electrodes (10-10 system) was performed. Interictal EEGs showed no epileptic discharges, but right frontal intermittent slowing. We recorded a right anterior temporal subclinical EEG seizure pattern (electrodes FT8, T8) without any clinical seizure symptoms, lasting 98 seconds. An ECD-SPECT tracer was injected during this EEG seizure pattern, 45 seconds after the onset of the EEG seizure pattern. The ictal SPECT with a technetium 99 m-labelled ethylcysteinate dimer (99mTc-ECD, Neurolite; BMS Pharma, Brussels, Belgium) was performed on a triple-head gamma camera (Multispect 3; Siemens, Erlangen, Germany) equipped with high-resolution collimators and showed a right fronto-mesial hyperperfusion. Three days later, repetitive clonic seizures of the left face were associated with right fronto-temporal EEG patterns of shifting, maximum between electrodes Fp2, F4, T8, F8 and FT8 (10-10 system). A second ictal ECD-SPECT tracer injection was performed 37 seconds after clinical seizure onset (left face twitching). This clonic seizure lasted for 102 seconds. This ictal SPECT showed a regional right frontolateral hyperperfusion at the posterior edge of the previous resection in the inferior frontal gyrus. For further evaluation, an interictal ECD-SPECT was performed. Subtraction of the first ictal (subclinical) and interictal SPECT showed a significant perfusion difference (23%) in the right mesial superior frontal gyrus (figure 2; blue colour). Subtraction of the second ictal (left face clonic seizure) and interictal SPECT showed a significant hyperperfusion (22%), predominantly at the dorsal margin of the former resection defect in the right lateral inferior frontal gyrus (figure 2; red colour).
Discussion
The SPECTs in our patient show highly localized hyperperfusion in two different regions associated with two different seizure semiologies from the same lobe. The SPECT subtraction technique is superior to conventional visual analysis for the localization of the seizure onset zone (Schauble and Cascino, 2003). Whereas the mesial fronto-polar hyperperfusion was clinically silent, the fronto-lateral hyperperfusion was associated with a contralateral clonic seizure of the face.
Ictal perfusion SPECT is an important imaging tool in the evaluation of patients considered for resective epilepsy surgery, especially in patients with non-lesional epilepsies (Duncan, 1997; Van Paesschen et al., 2007; Jayalakshmi et al., 2011). Its sensitivity and specificity are about 90% in TLE and 80% in extratemporal epilepsies (Spencer et al., 1995). The use of ictal subtraction SPECT -particularly when coregistered to MRI (as in this case)- was shown to improve sensitivity for the identification of an epileptogenic focus, and the combination of ictal subtraction SPECT with interictal PET may even provide better results (Matsuda et al., 2009; Desai et al., 2013). For ictal SPECT, early injection at seizure onset (less than 15-20 seconds after seizure onset) is highly likely to show regional hyperperfusion in the ictal onset zone (Lee et al., 2006; Van Paesschen et al., 2007). Relatively late injection in our patient may reflect spread of the epileptic activity, leading to false localization and more widespread hyperperfusion (Noachtar et al., 1998; Van Paesschen et al., 2000; Dupont et al., 2006). There are two explanations for divergent ictal SPECT results in the same patient: either the injection time was late and reflects spread of ictal epileptic activity or the patient has two independent seizure onset zones, with corresponding different EEG patterns and different semiology. However, the injection time was similarly late for both seizures. We cannot exclude a single seizure onset zone with different spread patterns leading to different semiology and ictal EEG patterns, ultimately reflected by variable SPECT hyperperfusion. The patient's epilepsy improved with change of medication and further surgery was not performed. Thus, an invasive EEG study was not justified to clarify the epileptogenic zone.
Simultaneous EEG during SPECT tracer injection was crucial for the interpretation of the SPECT. Without the EEG, the ictal character of the tracer injection would have been missed and interpretation would have been misleading. We conclude from our patient that subtraction of ictal and interictal SPECT is very sensitive in demonstrating the epileptogenic zone of epileptic seizures. Adequate interpretation of SPECT requires consideration of clinical symptomatology and simultaneous EEG.
Supplementary data
Summary didactic slides are available on the www.epilepticdisorders.com website.
Disclosures
None of the authors have any conflict of interest to declare.