Epileptic Disorders
MENUHot water epilepsy Volume 16, issue 1, March 2014
Hot water epilepsy (HWE) is a form of reflex epilepsy caused by contact with hot water. It is rarely described in European countries, whereas large series of patients have been reported in India and Turkey (Satishchandra, 2003). Most European patients present with a different form, probably related to immersion in water and not dependent on hot water; this form mostly affects children under two years of age (Ioos et al., 2000; Nechay and Stephenson, 2009). Recent evidence suggests that these two forms are clearly distinct, while many reports have considered these two forms to be a unique form of epilepsy (Nechay and Stephenson, 2009).
Seizures, mostly complex dyscognitive seizures, appear during contact with hot water, especially when poured over the head.
Pathogenesis is believed to result from a dysfunctional thermoregulation system in genetically susceptible patients, which is influenced by environmental factors (Shankar and Satishchandra, 1994; Satishchandra, 2003).
Differential diagnosis is possible through ictal video-EEG recordings, mostly to avoid confusion with other paroxysmal events. Few ictal recordings are reported in the literature, due to technical issues.
In this case study, we present a video-EEG recording of dyscognitive seizures induced by hot water in a nine-year-old boy and discuss the ictal EEG.
Case study
An eight-year-old boy presenting with seizures which only occurred during contact with hot water at home, especially when hot water was poured on his face (at approximately 40°C), was brought to our attention. Episodes lasted 30-60 seconds and the boy experienced malaise and a sensation of rising heat, after which he became pale with cyanosis of the lips, presented with oral automatisms, and was unable to speak. The seizure was followed by a period of confusion.
The boy was born after an uneventful pregnancy from a non-consanguineous marriage, delivery (by Caesarian section) was pre-term (35 weeks pregnancy). No perinatal problems were noted. Psychomotor development was normal. Neurological examination revealed clumsiness and dyspraxia. A neuropsychological evaluation was performed; IQ was within normal limits (80) and a specific learning disorder involving reading, writing, and calculation was diagnosed.
Neuroimaging was performed (CT and MRI); MRI revealed focal hyperintensity in deep white matter of the anterior region and in the peritrigonal area, interpreted as perinatal acquired damage.
The karyotype and CGH-Array were normal. Mutation analysis of the SCN1A gene resulted negative.
Interictal EEG was characterised by diffuse abnormalities, with slow activity in the anterior region, mixed with rapid activities (figure 1). During sleep, theta activity increased in amplitude and slow waves and rare bilateral anterior spikes appeared (figure 2).
During video-EEG monitoring, a seizure was recorded; 20 seconds after hot water (at approximately 40̊C) was poured on the boy's chest with a shower tube, he presented a generalised shudder, followed by a dystonic posture of the right limbs (particularly the upper limb). He appeared pale with cyanosis of the lips. He could speak and follow orders. After one minute, the episode ceased and the boy was able to report the end of the episode. On EEG, six seconds after the shuddering, a rhythmic theta activity appeared bilaterally in fronto-central and vertex regions, with an increase in amplitude during the episode; however, the presence of artefacts did not allow a clear interpretation of the remaining regions.
He was not treated with antiepileptic drugs, but seizures became very infrequent due to avoidance of exposure to hot water from the shower tube.
Three years later, he presented with complex partial spontaneous non-reflex seizures, consisting of a tingling ascending sensation (starting from inferior limbs), very similar to the sensation he experienced when in contact with hot water; followed by dizziness and visual complications. In addition, he described the initial sensation as a pleasant feeling and he reported the possibility of triggering a seizure through contact with something warm and thinking of water.
He was treated for one year with valproic acid and up to now is seizure-free.
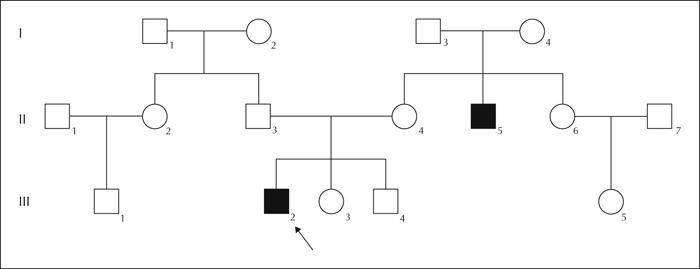
The uncle (37 years old), the brother of the proband's mother, had the same reflex epilepsy, from the age of seven, and had presented with complex partial seizures with secondary generalisation. He is now well-controlled by antiepileptic drugs (valproic acid and lamotrigine). Mutation analysis of the SCN1A gene resulted negative (figure 3).
Discussion
HWE has been included among the reflex epilepsies, according to the proposal of classification made by the ILAE in 2001; the stimulus consists of hot water being poured over the head, usually at a temperature of between 40 and 50°C (Satishchandra, 2003).
First described in New Zealand in 1945 (Allen, 1945), a large series of patients was reported by Satishchandra et al. (1988). In southern India, this kind of reflex epilepsy accounted for 3.6-3.9% of all epilepsy patients. Isolated cases have been described all over the world, but in European countries, this condition appears to be rare. Recently, many authors have suggested that these European cases usually present a different form of epilepsy, called “bathing epilepsy”, in which pathogenesis is connected to the immersion in water at a normal temperature, rather than contact with hot water (Nechay and Stephenson, 2009).
The variables that are considered to most likely account for the regional distribution are bathing habits (especially contact of the scalp with hot water and the temperature of the water), resulting in a combination of both cutaneous and heat stimuli (Ioos et al., 2000; Satishchandra, 2003; Yalcin et al., 2006), and genetic factors. A male:female ratio of approximately 2.5:1 is described (Satishchandra, 2003).
Seizures generally appear concomitantly upon contact with hot water, especially on the scalp region, but may also occur at a later stage during body bathing. Most of the patients experience complex partial seizures (67-80%), with or without secondary generalisation (Satishchandra et al., 1988; Bebek et al., 2001; Satishchandra, 2003; Yalcin et al., 2006).
Ictal semiology usually consists of a dazed look, a sense of fear, irrelevant speech, and visual and auditory hallucinations with complex automatisms. Seizures last from 30 seconds to three minutes. In a third of patients, generalised tonic-clonic seizures without focal features occur (Satishchandra et al., 1988; Satishchandra, 2003).
Self-induced seizures, described in other reflex epilepsies, have been reported in 10-30% of HWE patients (Bebek et al., 2006; Yalcin et al., 2006); these patients often described a pleasant feeling during seizures (Satishchandra et al., 1988; Bebek et al., 2001; Meghana et al., 2012) and in some cases compulsive self-induction was described (Bebek et al., 2001; Satishchandra, 2003).
Interictal EEG is usually normal, but in 15-20% of patients, diffuse abnormalities have been reported (Satishchandra et al., 1988), and rarely abnormalities involving temporal regions (Bebek et al., 2001; Yalcin et al., 2006). Only few reports have described ictal EEG activity, consisting mostly of focal temporal rhythmic slow-wave activity of high amplitude, with secondary generalisation (Satishchandra, 2003).
Pathogenesis is still unknown, but, according to the most probable hypothesis, seizures in HWE may represent a specific form of induced hyperthermia, caused by a dysfunctional thermoregulation system in genetically susceptible patients, with environmental influences, whereby a rapid increase in temperature occurring during bathing with hot water, involving the head, precipitates seizures (Shankar and Satishchandra, 1994; Satishchandra, 2003). Complex partial seizures associated with this form appear to be indicative of temporal lobe origin.
These hypotheses are supported by evidence of a history of febrile seizures in 11-27% of Indian patients and 9.5% in a Turkish study (Satishchandra et al., 1988; Bebek et al., 2001; Meghana et al., 2012), the absence of lesion on brain MRI and autoptic findings (Shankar and Satishchandra, 1994; Szymoniwizc and Meloff, 1978; Bebek et al., 2001; Meghana et al., 2012), and preliminary studies that demonstrate functional involvement of mesial temporal structures and hypothalamus, as indicated by ictal hypermetabolic uptake (Satishchandra, 2003).
In many studies, a positive family history of epilepsy (reported in 7-44% of patients) is emphasized, supporting genetic predisposition (Bebek et al., 2001; Satishchandra, 2003; Yalcin et al., 2006); in 10% of patients, a family history of HWE is reported (Bebek et al., 2001). Studies on HWE family clusters have identified two possible genetic loci, one on chromosome 10 (10q21.3-22.3) and one on chromosome 4 (4q24-q28) (Ratnapriya et al., 2009a; Ratnapriya et al., 2009b).
Good control of seizures is usually obtained by avoiding hot water, however, in patients who still have seizures, prophylactic use of bendoziadepines (clobazam) before contact with hot water has been suggested with good results (Satishchandra, 2003; Meghana et al., 2012). Approximately 16-38% of patients develop spontaneous non-reflex seizures (Satishchandra et al., 1988; Satishchandra, 2003). In these cases, antiepileptic drugs are necessary. The development of non-reflex seizures in HWE patients has been proposed as evidence of hyperthermic kindling in humans (Satishchandra, 2003).
To our knowledge, this is the first case of HWE described in western countries, with a positive family history of HWE, in which genetic testing was performed. However, no deletion or duplication was identified using CGH-Array in the patient or affected relative, and SCN1A gene mutation analysis, which was performed based on the hypothesis that seizures were caused by a form of induced hyperthermia, was negative. In this family, the evidence of genetic predisposition appears to be specific to HWE, since no other epilepsy syndrome or febrile seizures were reported.
A typical case of HWE is characterised by a combination of clinical and EEG characteristics and seizures are triggered by a specific combination of sensory stimuli, specific to each patient. Seizures may initially be avoided simply by environmental precautions (as described and suggested in the literature), but this did not prevent the appearance of non-reflex seizures, resulting in the necessity to prescribe antiepileptic drugs, with good control of seizures.
Self-induced seizures, which are frequently reported (Bebek et al., 2006; Yalcin et al., 2006), were confirmed in this case.
Few ictal video-EEG recordings are reported in the literature, due to difficulties in provoking such reflex seizures in laboratory conditions. In this study, we report ictal EEG accompanied by video sequences of a patient experiencing a partial seizure, arising from the anterior regions of both hemispheres. The semiology of this seizure appeared to be characterised by shuddering, followed by dystonic limb posture, mild delay, and difficulty in answering questions, without clear loss of contact, and vegetative symptoms. The electroclinical characteristics of the seizure are consistent with frontal involvement, while temporal regions cannot be clearly evaluated due to technical complications. Previously reported ictal recordings of HWE have demonstrated a temporal involvement for seizures (Satishchandra, 2003).
Epileptic seizures in a child with clinical semiology of shuddering and atypical presentation have been reported with a cingulate gyrus origin (Jahodova et al., 2012).
HWE is a rare form of reflex epilepsy, usually reported in Eastern countries. The Caucasian patient described herein showed clinical characteristics and long-term outcomes similar to this typical form of reflex epilepsy.
Disclosures
None of the authors have any conflict of interest to disclose.