Epileptic Disorders
MENUEarly-life epileptic encephalopathy secondary to SZT2 pathogenic recessive variants Volume 18, issue 2, June 2016
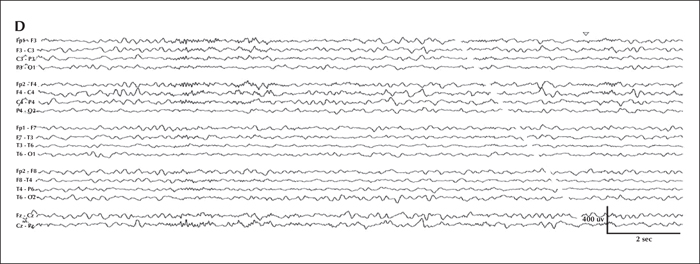
Figure 1
Serial EEG from initial presentation and the latest follow-up visit. Overnight video-EEG was performed during hospital admission for breakthrough seizures within two weeks of initial epilepsy diagnosis (2.5 months old) and captured an electroclinical tonic seizure characterized by unresponsiveness and staring for six seconds, followed by asymmetric (left>right) limb extension with vibratory stiffening. Electrographically, at onset (A), there was diffuse attenuation, subsequently maximal at the vertex, followed by rhythmic discharges that gradually spread to the bilateral central region; on the right more than the left (B). Sleep background at 2.5 months old (C) was significant for symmetric sleep spindles and intermittent epileptiform discharges maximal in the central vertex region. The most recent EEG was performed at 3 years of age (D) and background activity during sleep was significant for subtle relative left hemispheric attenuation, occasional multifocal epileptiform discharges, and asymmetric sleep spindles and vertex waves, higher in amplitude on the right.
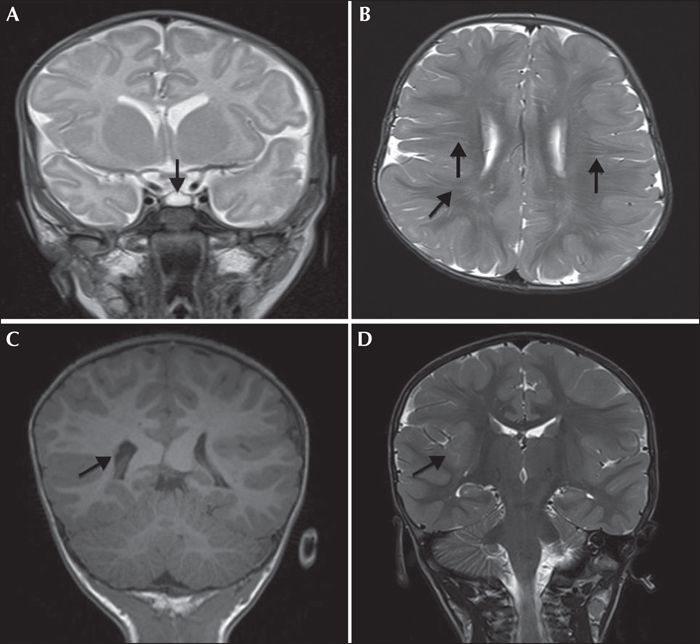
Figure 2
MRI of the patient at different time points. (A) MRI performed at 2 months of age showing Rathke's cleft cyst (arrow) and asymmetric hemisphere size (left cerebrum smaller than right). (B) MRI performed at 11 months of age showing linear, radially-oriented T2 hyperintensities within the white matter with unclear significance (arrows). (C, D) MRI performed at 2 years of age shows right periventricular heterotopia (arrow in C) and abnormal perisylvian gyral configuration (C and arrow in D).

