Epileptic Disorders
MENUCorpus callosotomy in a patient with startle epilepsy Volume 15, issue 1, March 2013
epd.2013.0553
Auteur(s) : Nicolás Garófalo Gómez1 nicogaro72@gmail.com, Ana Paula Hamad2, Murilo Marinho2, Igor M Tavares2, Henrique Carrete Jr3, Luís Otávio Caboclo2, Elza Márcia Yacubian2, Ricardo Centeno2
1 Neuropediatric Department, Cuban Institute of Neurology and Neurosurgery, Havana, Cuba
2 Department of Neurology and Neurosurgery
3 Department of Imaging Diagnosis, Hospital São Paulo, Universidade Federal de São Paulo, Brazil
Correspondence. Nicolás Garófalo Gómez Neuropediatric Department, Cuban Institute of Neurology and Neurosurgery, 29 y D, Vedado, Plaza, Havana, CP 10 400, Cuba
Startle epilepsy (SE) is a type of reflex epilepsy in which epileptic seizures are precipitated by a sudden and surprising, usually auditory, stimulus (Panayiotopoulos, 2010). The startle response is brief and consists of axial tonic posturing, frequently causing falls which can often be traumatic (Yang et al., 2010).
The aetiology, type of structural brain abnormality, type of clinical seizure, and EEG features in patients with SE are variable (Yang et al., 2010). Prognosis is often poor. There is no established drug of choice and treatment with antiepileptic drugs (AEDs) is usually unsatisfactory (Panayiotopoulos, 2010). Some reports suggest that surgical intervention might be effective in patients with SE associated with infantile hemiplegia (Oguni et al., 1998; Martinez-Mañas et al., 2004).
The aim of this report was to present a case of SE, with normal magnetic resonance imaging (MRI), in which the patient underwent surgical treatment by corpus callosotomy (CC), leading to seizure freedom.
Case study
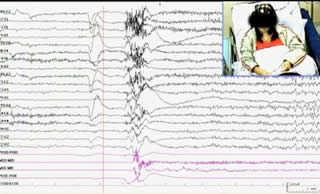
A 17-year-old girl presented with SE and seizures refractory to medical treatment. Her birth was uneventful and her psychomotor development was largely unremarkable until 2 years of age, when she started to have tonic seizures at a frequency of three to four per day. She had been suffering with several types of seizure (tonic, atonic, and focal with sensory-motor symptoms), refractory to various AEDs. Almost all seizures were provoked by sudden unexpected sounds (never by other sensory modalities) and were characterised by extension of the four extremities with elevation of the upper limbs and drop attacks. At age 10 years, she showed behavioural disturbances and had a suicide attempt. Presurgical evaluation revealed no neurological deficits, moderate mental retardation, normal brain MRI, and no interictal or ictal lateralised or localised signs on video-polygraphic recordings (figure 1A and video sequence 1). The patient's quality of life (QOL) was greatly impaired by intractable seizures.
In the absence of signs of focal epileptogenesis and in order to control drop attacks, CC was the indicated surgical treatment. During surgery, access to the interhemispheric fissure was difficult due to a complex venous distribution at the midline as well as the position of the head, with the sagittal sinus parallel to the floor, causing poor illumination of the bottom of the surgical field. These technical aspects made it difficult to perform a two-third anterior callosotomy. There was a small infarct in the right medial frontal lobe, a surgical complication probably related to hemispheric retraction (figure 2).
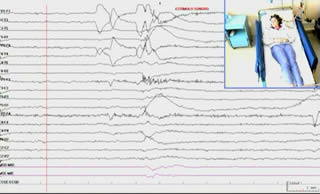
After one year of follow-up, remission of all seizure types was observed (Engel Class IA) on treatment with AEDs. There was remarkable improvement of daily life activities. On physical examination, the patient presented with mild central left leg paresis. A new video-polygraphic recording was obtained. No changes in morphology, incidence, or distribution of interictal discharges were observed. However, she did not present with any seizures, even in the presence of stimuli with sudden arousal (figure 1B and video sequence 2).
Discussion
The decision to refer our patient for CC was taken as an alternative to AED treatment, with the aim of reducing drop attacks and trying to improve the patient's QOL, considering that no brain lesion was detected in presurgical MRI studies. A mid-central callosotomy was performed instead of a two-third anterior callosotomy due to anatomical and technical difficulties observed during the procedure.
The possible cerebral areas implicated in epileptogenesis of SE include prefrontal, supplementary motor, and sensorimotor cortical areas. However, the exact mechanism underlying seizure provocation has yet to be defined (Saeki et al., 2009).
CC was first introduced as a surgical technique for the treatment for epilepsy in 1939. It is often used to treat atonic, clonic, myoclonic, and generalised tonic-clonic seizures. The best results have been consistently observed with atonic seizures; however, some success has also been shown with tonic and secondary generalised seizures (Clarke et al., 2007). CC is an effective treatment option for intractable generalised seizures that are not amenable to focal resection. When considering this procedure, the treating physician must thoroughly assess the expected benefits, limitations, likelihood of residual seizures, as well as the risks of the procedure, and explain these to the patient, family, and other caregivers (Tanriverdi et al., 2009).
Considering the costs and benefits of surgery, our patient presented with mild left crural paresis due to a small postsurgical cerebral infarction; however, she has been completely seizure-free since surgery.
We found no reports in the literature on the use of CC for the treatment of patients with SE without demonstrable lesion on MRI. This treatment option was chosen in our case in order to try to diminish the severity of tonic seizures. Surprisingly, the patient became free of all seizures.
The question remains whether this excellent outcome was due to the CC, the brain injury related to the small brain infarction, or the sum of these two events. Since the main field of the interictal and ictal epileptiform discharges was located in central regions, the same area involved in the physiopathology of SE, we cannot rule out the hypotheses that the brain infarct played a role in the postsurgical outcome in our case.
Kwan et al. (2000) reported a case with Lennox-Gastaut syndrome with auditory-induced generalised atonic or tonic seizures in which the patient was treated with CC, leading to a 60% decrease in seizure frequency. Our patient was seizure-free one year after surgery, but the interictal epileptiform discharges persisted over central regions. However, there is enough evidence to support the hypothesis that the CC contributed to the good postoperative outcome.
Despite the limited scientific evidence provided by a case study, this report shows that CC may be considered for patients with SE and tonic seizures, in the absence of focal lesions amenable to surgery.
Legends for video sequences 1 Video sequence 1 Presurgical video-EEG. A generalised tonic reflex seizure was provoked by a sudden unexpected sound; the clinical-electrographic seizure lasted for 10 seconds and postictal EEG showed central, slow rhythm in addition to interictal discharges. 2 Video sequence 2 Postsurgical video-EEG. A sudden unexpected sound was produced, but no startle seizure was triggered. The EEG was also unremarkable. Key words for video research on www.epilepticdisorders.com
- Syndrome: reflex epilepsy
- Etiology: unknown
- Phenomenology: startle response; tonic seizure; atonic seizure (drop attack)
- Localization: not applicable
Acknowledgements and disclosures
This work was supported by the ALADE (Academia Latino Americana de Epilepsia) and the ILAE (International League Against Epilepsy).
None of the authors has any conflicts of interest to disclose.