Epileptic Disorders
MENUCan ACTH therapy improve the long-term outcome of drug-resistant frontal lobe epilepsy? Volume 16, issue 2, June 2014
Frontal lobe epilepsy (FLE) is the second commonest focal epilepsy in children after temporal lobe epilepsy, accounting for 20-30% of partial epilepsies, despite the lack of information regarding its true incidence (Manford et al., 1992). Although FLE is usually cryptogenic in childhood, it is often complicated by neuropsychological impairment, behavioural disorders, and drug resistance (Braakman et al., 2011). A possible cause of the unfavourable evolution of childhood FLE is the likelihood that the condition will worsen at different disease stages due to rapid diffusion of epileptogenic discharges (secondary bilateral synchrony [SBS]). In these cases, seizures become increasingly frequent, resulting in a global worsening of epilepsy.
The use of adrenocorticotropic hormone (ACTH) is generally accepted as the treatment for West syndrome. According to the guidelines of the American Academy of Neurology and Child Neurology Society, ACTH is effective for the short-term treatment of infantile spasms (Go et al., 2012) and also in patients with infantile spasms without hypsarrhythmia (Oguni et al., 2005).
ACTH or steroids have also been used for patients with other forms of medically intractable epilepsy. In a retrospective study of 15 patients with refractory generalised seizures treated with ACTH, short-term effectiveness was reported in most cases, but also a high percentage of medium and long-term seizure recurrence (Okumura et al., 2006).
In the present study, we report our experience of patients with frontal lobe seizures, namely tonic versive seizures with or without drop attacks. In addition to tonic versive seizures, some of these patients during disease evolution developed a clinical picture of atypical absences and drop attacks, concomitant with EEG features of SBS. These patients were administered ACTH treatment with good outcomes. On the strength of this initial experience, 4 other patients, who had developed frontal lobe seizures with tonic versive seizures complicated by atypical absences and drop attacks, received prompt ACTH treatment.
Material and methods
Patients were recruited for an add-on trial during clinical practice and the data, collected prospectively over time, was analysed retrospectively. The study group comprised 6 patients recruited between 1985 and 2011 by one of the authors (GG). Patients were selected according to the following inclusion criteria:
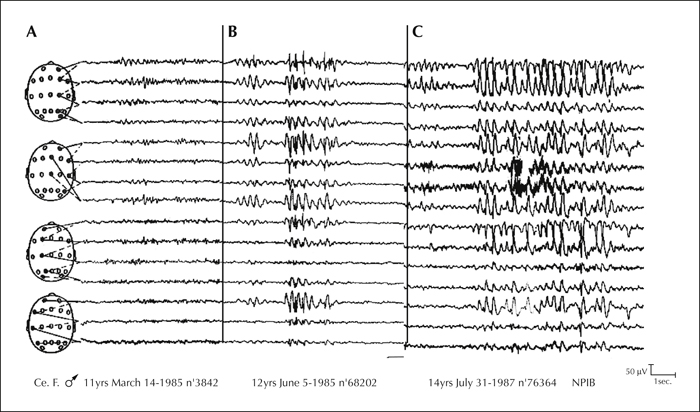
- (1)Patients who had received a diagnosis of epilepsy with frontal lobe seizures (FLE) according to the 1981 and 1989 ILAE classification of epilepsies and epileptic syndromes (Commission, 1981; Commission, 1989). Simple partial seizures were generally short, with prominent tonic or postural motor manifestations. Complex gestural automatisms were frequent at onset. Atypical absences and drop attacks appeared later during the evolution, concomitantly with the appearance of SBS on EEG (figure 1A, 1B, 1C). Video-polysomnographic recordings showed a broad spectrum of seizures occurring both upon awakening and during sleep (figure 1A, 1B, 1C);
- (2)Absence of brain lesions on MRI;
- (3)Normal blood and cerebrospinal fluid tests, chromosome analysis, and screening for metabolic and autoimmune disorders;
- (4)Drug resistance to at least two antiepileptic drugs (AEDs), given alone or in combination;
- (5)Negative neurological examination;
- (6)Normal psychomotor development;
- (7)Presence of parents or legal guardian, who had recorded seizures in a diary.
Seizure frequency, before and after treatment, was calculated on the basis of the number of seizures/month recorded in the diary. The frequency and type of seizures was registered based on EEG recordings during wakefulness/sleep at baseline, at the end of target therapy titration, after 6 months of treatment, and at the end of follow-up. Seizures were classified according to the International League Against Epilepsy and the revised classification of seizures (Commission, 1981). Since the dose and duration of ACTH should be minimised in order to avoid serious adverse effects, we chose treatment with low-dose ACTH since higher doses were reported to be as effective (Hrachovy et al., 1994; Yanagaki et al., 1999); this was subsequently confirmed by Go et al. (2012).
The ACTH dose used was 0.01 mg/kg/day i.m. for 2 weeks in all patients, followed by tapering for 6 weeks, except for Patient 4 who continued the cycle with a progressive dose reduction over a total of 4 months. The effects of ACTH were assessed during short-term (at the end of the 6-week ACTH treatment), medium-term (at 6 months after the end of treatment), and long-term (at 12 months after the end of treatment) periods.
In agreement with Okumura's evaluation criteria (Okumura et al., 2006), the short-term outcomes of ACTH were classified into three categories: effective, in the case of seizure cessation; partially effective, in the case of persistent seizures with a >50% reduction in frequency; and ineffective, in the case of persistent seizures with a <50% reduction in frequency.
The medium and long-term outcomes were classified into the following three categories: excellent, with a complete disappearance of seizures; good, with persistent seizures and a >50% reduction in frequency;and poor, with persistent seizures and a <50% reduction in frequency. The demographic characteristics of patients are listed in table 1.
Results
As a whole, at short-term follow-up, ACTH treatment was effective for all types of seizures in 5/6 patients and ineffective in the remaining patient. The results are summarised in table 1.
In detail, the seizure types that responded to ACTH included: atypical absences (in 5/6 cases), tonic versive seizures (in 4/5 cases), drop attacks (in 2/2 cases), and tonic seizures and complex partial seizures (in 1/1 case). In addition, all patients who were seizure-free at the end of ACTH treatment maintained an excellent outcome, remaining seizure-free at the end of follow-up.
Table 2 summarises the EEG and outcomes after add-on AED treatment. In the ACTH group, the EEG normalised at the end of follow-up in 3/6 patients; a focalization of abnormalities was noted in another 2 patients with a disappearance of the SBS in 5/6 patients. One patient was a non-responder with persistent SBS and tonic versive, generalised tonic-clonic seizures, and atypical absences. The number of AEDs was reduced at the end of follow-up in 5/6 patients.
Discussion
Frontal lobe epilepsy accounts for 20-30% of all partial epilepsies (Manford et al., 1992). Most cases of FLE are drug-resistant and treatment is mainly surgical. The outcome of focal neocortical resection varies, with between 36 and 76% of patients becoming seizure-free (Spencer and Huh, 2008). Most of the literature on FLE comprises surgical reports whereas information on drug management is scant.
AEDs, vagal nerve stimulation (VNS), the ketogenic diet (KD), and rarely multiple subpial transection (MST) may be valid alternative therapies for FLE patients not eligible for surgery. With VNS, a 50% reduction in seizure frequency is achieved in around a third of FLE patients, but few become seizure-free (Morris and Mueller, 1999). A significant reduction of seizures has been reported after MST (Spencer and Huh, 2008), while KD, a high-fat low-carbohydrate diet, is used as a second-line treatment for children with medically intractable FLE. A recent randomised controlled trial reported a >50% seizure reduction in 38% of children with drug-resistant FLE (Neal et al., 2008).
An add-on AED leads to complete seizure control in 17% of patients with chronic forms of FLE (lasting >five years) and a 50 to 90% reduction of seizure frequency in 25% of cases (Luciano and Shorvon, 2007). Zonisamide, levetiracetam, lamotrigine, topiramate, and gabapentin have all proved to be effective add-on medications in patients with intractable FLE (French et al., 2004; Oldani et al., 2005; Verrotti et al., 2007).
The use of ACTH as treatment for medically intractable seizures was first reported in 1950. Since ACTH proved effective for the treatment of infantile spasms, the hormone has long been the first choice medication for West syndrome. ACTH has also been successfully used to treat epileptic spasms without hypsarrhythmia (Oguni et al., 2005)and Landau-Kleffner syndrome (Lerman et al., 1991). The role of steroids in other forms of epilepsy, such as Lennox Gastaut syndrome, severe myoclonic epilepsy in childhood, myoclonic or myoclonic-astatic seizures (drop attacks), atypical absences, and other epileptic syndromes, is less well-defined (Gupta and Appleton, 2005).
Steroids are administered as add-on drugs with other AEDs, such as sodium valproate, topiramate, and lamotrigine, often during acute attacks (e.g. non-convulsive status epilepticus), but few studies have compared corticosteroids and ACTH in the treatment of epilepsy in children (Gupta and Appleton, 2005). Snead et al. administered ACTH and prednisolone to 116 patients, 64 with drug-resistant epilepsy (mainly myoclonic seizures) not associated with West syndrome, and reported a 74%-positive outcome in ACTH-treated patients (Snead et al., 1983). Okumura et al. (2006) studied the effect of ACTH therapy in 15 children with medically intractable epilepsy. Thirteen children became seizure-free but six of them experienced a recurrence of seizures in the three months after ACTH withdrawal. One 8-year-old patient with FLE had a good short-term response but his medium and long-term outcome was poor. Sinclair (2003) found that 46% of drug-resistant children in his cohort became seizure-free, while 40% had a significant reduction in seizure frequency after prednisone therapy. Verhelst et al. (2005) reported seizure freedom in 25% of their cases, a >50% seizure reduction in 11%, and a <50% seizure reduction in 11%. Steroids have also been used to treat epilepsia partialis continua (Olson et al., 2002; Shahar et al., 2002), and a 17-year-old girl with severe status epilepticus of frontal lobe origin was successfully treated with corticosteroids (Akanuma et al., 1998).
These findings indicate that ACTH could be considered an alternative treatment for epilepsies other than infantile spasms. On this basis, we chose ACTH to treat our drug-resistant FLE patients.
The decision to administer ACTH therapy was based speculatively on the apparent similarities with epileptic encephalopathy. In fact, these patients were affected by a focal epilepsy with frontal lobe seizures since their epilepsy started with frontal seizures and the EEG showed frontal-onset focal discharges. Later during disease evolution, because of SBS, the EEG discharges became bifrontal, seizures became more and more frequent, drop attacks appeared, and there was deterioration of mental ability. This severe evolution of FLE with the appearance of SBS on the EEG has already been described by Beaumanoir and Mira (2003), and should be distinguished from Lennox Gastaut syndrome and continuous spike and waves during sleep syndrome. Our study showed that ACTH treatment was associated with a disappearance of seizures in 5 of 6 children with refractory cryptogenic FLE. The hormone was administered at different stages of disease evolution when SBS appeared and seizures became more frequent.
The most interesting aspect of our study was the long-term outcome of our patients. Whereas the few studies in the literature on ACTH or steroid use in intractable generalised epilepsies report a long-term recurrence of seizures in about half the patients responding to treatment, our patients remained seizure-free in the long-term. In addition, none of our patients had ACTH-induced adverse effects requiring suspension of treatment. Speculatively, one may assume that these five patients had an age-dependent variant of FLE, evolving towards spontaneous remission after the initial phase. In any case, ACTH proved to facilitate a favourable evolution in our patients, in line with its success against intractable or difficult-to-treat epilepsies other than infantile spasms.
In conclusion, despite the small cohort of treated patients, our study demonstrates that ACTH may represent an effective treatment for FLE, a difficult-to-manage form of epilepsy that often requires AED polytherapy. ACTH appears to be particularly effective if administered early, when FLE is associated with the onset of EEG signs of SBS. Further and larger double-blind prospective studies are required to confirm our initial findings.
Disclosures
The authors state no conflict of interest and have received no payment in preparation of this manuscript. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.