European Journal of Dermatology
MENUSuccessful treatment of psoriatic arthritis associated with adrenal hypoplasia congenita using infliximab Volume 28, issue 5, September-October 2018
Figures
Psoriatic arthritis (PsA) is inflammatory arthritis associated with psoriasis, which often leads to impaired function and reduced quality of life [1]. Adrenal hypoplasia congenita (AHC) is a rare congenital disorder typically presenting with primary adrenal insufficiency (PAI) during infancy [2]. PsA associated with AHC is extremely rare, and limited information is available in the English literature. Moreover, efficient and safe therapeutic strategies for this combination have not been established. Here, we report a case of PsA associated with AHC, successfully treated with infliximab.
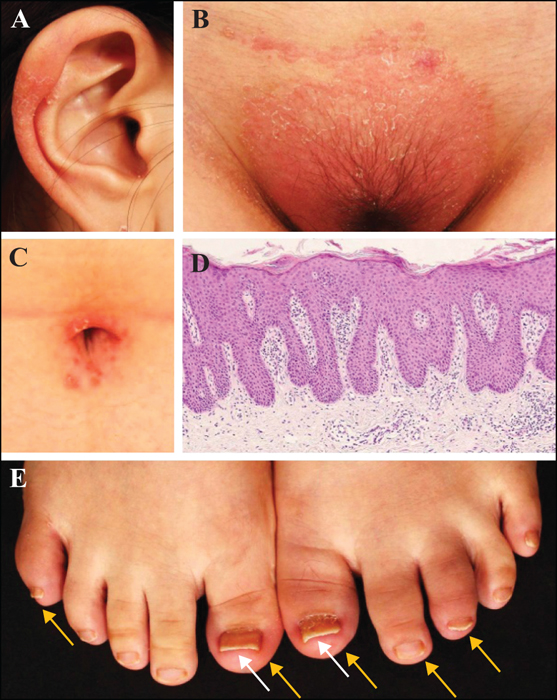
A 21-year-old Japanese woman with a five-year history of psoriasis was referred to our hospital. She showed typical clinical and pathological features of psoriasis (figure 1A-D). She also had swollen toes (figure 1E) and arthralgia of the knees for one year. The laboratory results were as follows: rheumatoid factor and anti-cyclic citrullinated peptide antibodies were negative, erythrocyte sedimentation rate (ESR) of 54 mm/h (reference: <15 mm/h), C-reactive protein at 32.5 mg/L (reference: <3.0 mg/L), and matrix metalloproteinase-3 at 179.2 ng/mL (reference: 1.25-20.0 ng/mL). The patient did not carry HLA-B27 alleles. Based on these findings, she was diagnosed with PsA. The psoriasis area and severity index (PASI) score was 5.4, while the 28-joint disease activity score based on ESR was 5.5, which was considered to represent a high level of disease activity.
It should be noted that the patient had been diagnosed with AHC in early infancy, followed by a diagnosis of hypergonadotropic hypogonadism in adolescence. She had no family history of AHC. She had been treated with oral hydrocortisone (20 mg/day), fludrocortisone (0.075 mg/day), and oestrogen-progestogen replacement therapy, and there were no symptoms of adrenal failure.
Infliximab was initiated at 5 mg/kg along with methotrexate (4 mg/week). Rapid and significant improvements were noted two weeks after the initial infliximab injection, and her American College of Rheumatology (ACR) Criteria score indicated an ACR50 response. After the second injection (Week 6), the number of tender and swollen joints decreased from 2 to 0 and 7 to 0, respectively. Subsequently, she achieved an ACR70 response and PASI-100 response at 14 weeks. Although she received infliximab for more than two years, no adverse events were observed throughout the treatment course.
Here, we present a case of PsA associated with AHC, which was successfully treated with infliximab. This case offers two important clinical suggestions.
First, PsA can occur with AHC. Because of the rarity of AHC, the precise rates of AHC with rheumatic diseases, such as PsA, have not been well established. However, it was recently reported that PAI was significantly associated with PsA. A population-based case-control study was conducted to investigate a potential association between PAI and PsA. It revealed that the adjusted odds ratio was 3.48 (95% CI: 1.54-7.81; p = 0.003) for PsA in individuals with PAI [3]. This rare combination of PsA and PAI may be biologically plausible. In patients with PAI, the blood cortisol level under conditions of stress is low [4]. Previous studies have shown that cortisol suppresses tumour necrosis factor (TNF)-α expression by affecting gene transcription and post-translational events [5]. In addition, synovial samples from patients with PsA showed marked expression levels of proinflammatory cytokines including TNF-α [6]. Thus, we hypothesized that adrenal insufficiency in PsA patients might fail to suppress TNF-α levels in the synovium and synovial fluid, and may consequently result in severe joint damage.
Second, infliximab can be a treatment option for PsA patients with AHC. According to evidence-based treatment recommendations for PsA, anti-TNF-α agents should be prescribed as initial treatment for those with active articular disease [7, 8]. However, there are limited data to guide treatment for PsA patients with PAI. In our case, AHC was stable with hormone replacement therapy, therefore we selected infliximab with consideration of the severity of the articular disease. Consequently, the patient achieved marked clinical improvement without a harmful influence on AHC. To the best of our knowledge, this is the first report to show the efficacy and safety of infliximab for PsA associated with PAI and AHC.
In conclusion, PsA can occur with AHC, and infliximab may be used as treatment for PsA patients with AHC. Although a long-term follow-up and further studies are required to clarify the safety of infliximab, our experience, in this case, provides evidence of successful treatment for PsA patients with PAI.
Disclosure
Financial support: none. Conflict of interest: none.