Epileptic Disorders
MENUMeasurable outcomes for pediatric epileptic encephalopathy: a single-center experience with corticosteroid therapy Volume 23, numéro 1, February 2021
- Mots-clés : epileptic encephalopathy, corticosteroids, seizure frequency, EEG, sleep, cognition
- DOI : 10.1684/epd.2021.1247
- Page(s) : 111-22
- Année de parution : 2021
Objective
Corticosteroids are commonly used to treat refractory epilepsy in children, but the heterogeneity of the population and lack of standardized outcome measures have limited understanding of their effectiveness. We conducted a single-center study of corticosteroids for epileptic encephalopathy to (a) identify domains for measurement and estimate potential effect sizes, (b) characterize heterogeneity, and (c) identify outcomes that may need better tools for measurement.
Methods
In this retrospective single-center cohort study, children with epileptic encephalopathy (excluding infantile spasms) were treated with a standardized course of oral dexamethasone or IV methylprednisolone. Long-term video electroencephalography (EEG) was assessed via novel ordinal scales for five features: seizure semiology/burden, epileptiform activity, slowing, organization, and sleep architecture. We abstracted parental assessment of functional domains (i.e., cognition) from the medical records. Pre-treatment and post-treatment EEG features, functional domains, and treatment regimens were compared.
Results
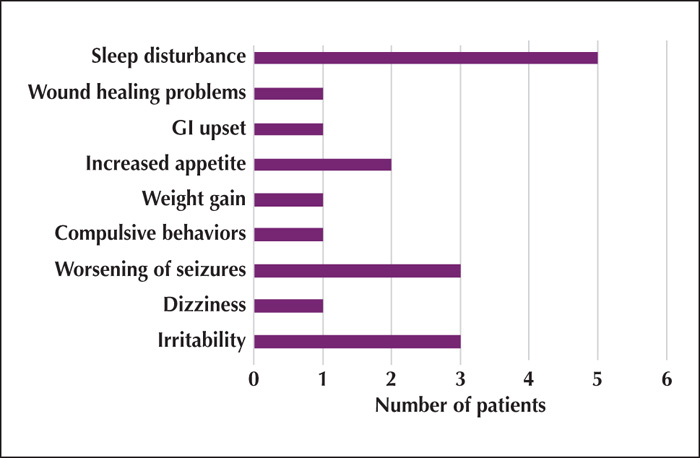
Thirty-five children with refractory epilepsy were included. Overall, 16/35 (46%) of individuals had a >50% reduction in seizure frequency from the pre-treatment EEG to the initial post-treatment EEG. In particular, tonic seizures (in a subset of 23 children) were reduced (24-hour tonic seizure count pre-treatment was 8 [4-13] and 3 [1-5] post-treatment EEG#1, p=0.04). For follow-up post-treatment EEGs, there was: (1) better formation of sleep spindles (37% normal pre-treatment to 63% normal post-treatment; p=0.04); and (2) improvement in parental reported cognition (in 43%). Improved cognition was the only outcome that differed between the dexamethasone and methylprednisolone treated groups (58% for dexamethasone [n=11/19] vs. 25% for methylprednisolone [n=4/16]; p=0.03).
Significance
Large studies should be powered to detect reductions in seizures (particularly tonic as we identified a 2.6-fold reduction), improved EEG organization, and improved sleep architecture (21 percentage points). Cognitive improvements following steroid treatment, reported by parents, should be quantified and fully characterized in future work.