Epileptic Disorders
MENUPost-encephalitic epilepsy in childhood: results from a prospective cohort study Volume 23, numéro 1, February 2021
- Mots-clés : central nervous system, paediatric, outcome, epilepsy, encephalitis
- DOI : 10.1684/epd.2021.1251
- Page(s) : 133-42
- Année de parution : 2021
Objective
To investigate whether it is possible to predict outcome of post-encephalitic epilepsy based on findings during the acute phase of disease.
Methods
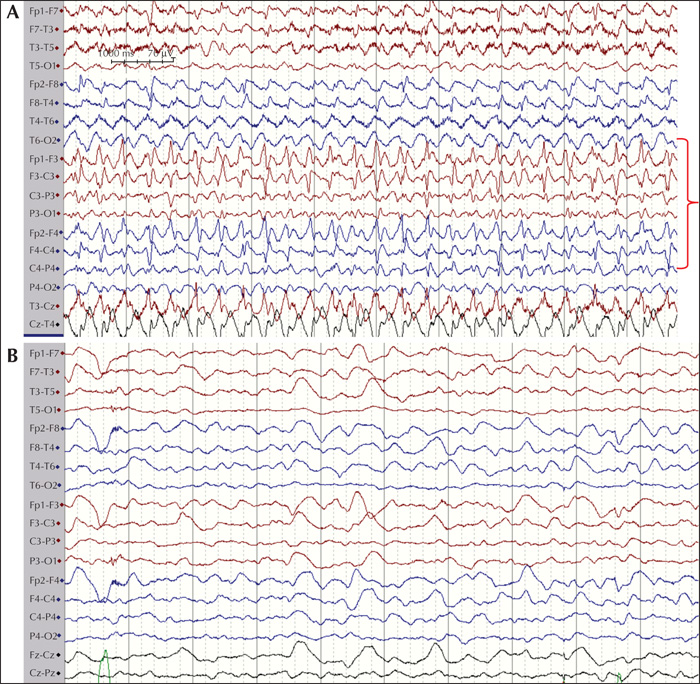
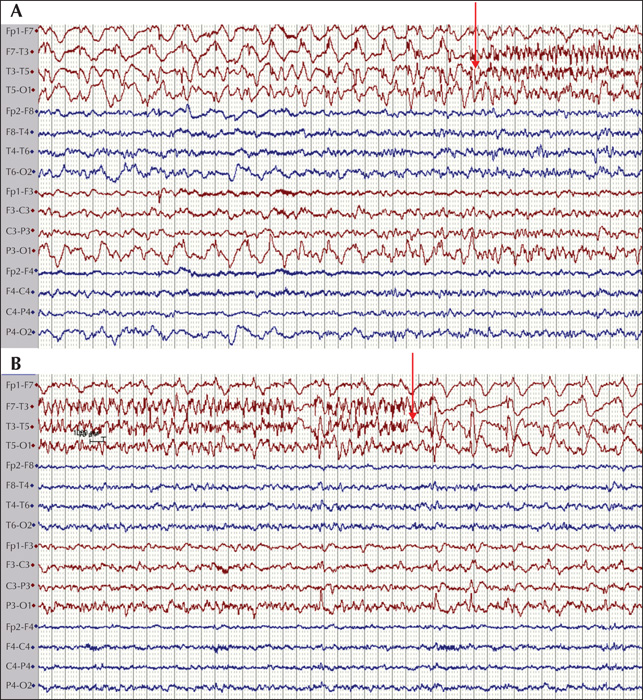
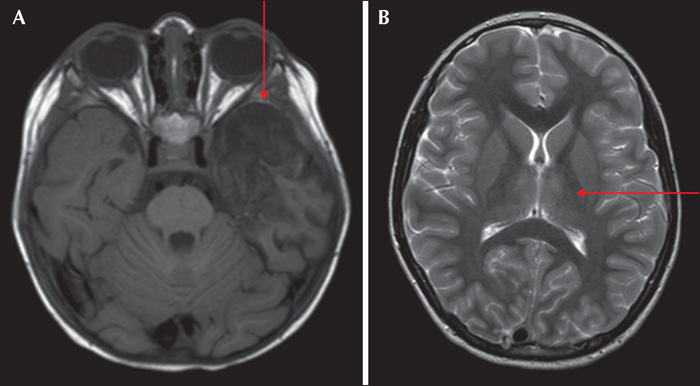
Children (28 days to 17 years) diagnosed with acute encephalitis at Karolinska University Hospital between 2011 and 2016 were included in this study (n=89). They were examined clinically, with repeated electroencephalographic examinations and analysis of cerebrospinal fluid during the acute illness. Thereafter, patients were followed up to 24 months and evaluated for post-encephalitic epilepsy. Variables determined during the acute illness were used to predict the development of post-encephalitic epilepsy: electroencephalographic parameters, cerebrospinal fluid parameters, aetiology and clinical parameters. Fisher's exact test was used to estimate any predictors of epilepsy among the acutely measured parameters.
Results
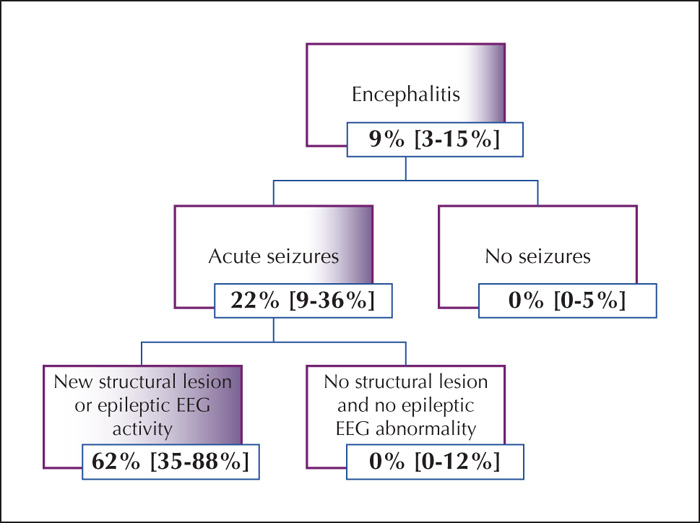
The prevalence of post-encephalitic epilepsy was 9% (n=8) at 24 months. Of these, 3/8 responded to monotherapy with antiepileptic drugs and 5/8 required two or more and 3/8 were medically refractory at 24 months. Presence of acute seizures during admission, epileptic activity on electroencephalographic recordings and new-onset structural lesions demonstrated a significant association with development of post-encephalitic epilepsy (p<0.03) with an odds ratio greater than 5. Using the three above-mentioned parameters, we designed an algorithm to predict cohorts of patients with increased risk of developing post-encephalitic epilepsy. Moreover, patients who developed post-encephalitic epilepsy had a longer duration of hospital admission and longer care in intensive care units in comparison to those who did not.
Significance
This study demonstrates that the risk of developing post-encephalitic epilepsy was mainly seen among patients with acute seizures, epileptic encephalographic activity in the acute setting or new-onset structural lesions. A simple algorithm could be used to predict the risk of post-encephalitic epilepsy.