Epileptic Disorders
MENUPost-encephalitic epilepsy in childhood: results from a prospective cohort study Volume 23, numéro 1, February 2021
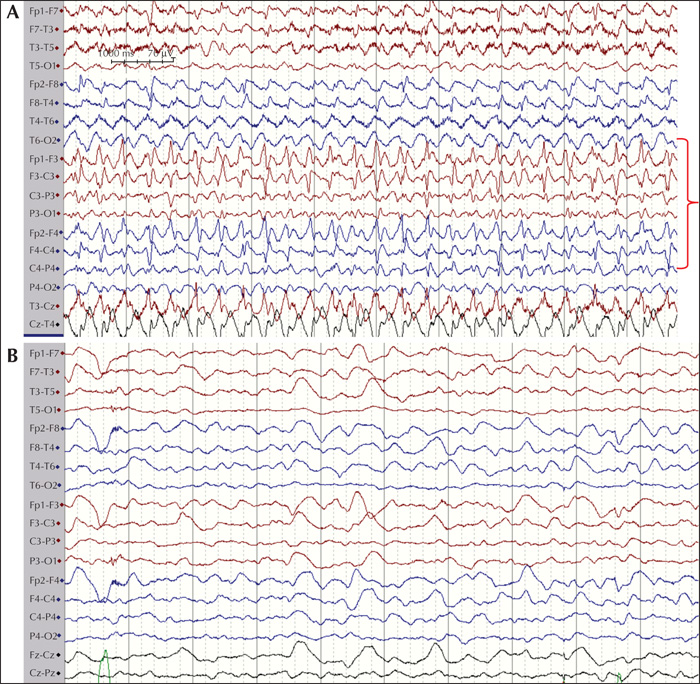
Figure 1
EEG from a nine-year-old female with Hashimoto's encephalitis. On admission to the hospital, the patient presented with reduced consciousness and minor twitching. She previously had several convulsive seizures. (A) Rhythmic spiking could be seen on the EEG indicating non-convulsive status epilepticus (marked in red). (B) The patient was initially sedated, and repeat EEG the next day showed mainly an encephalopathic picture (partly sedation effect).
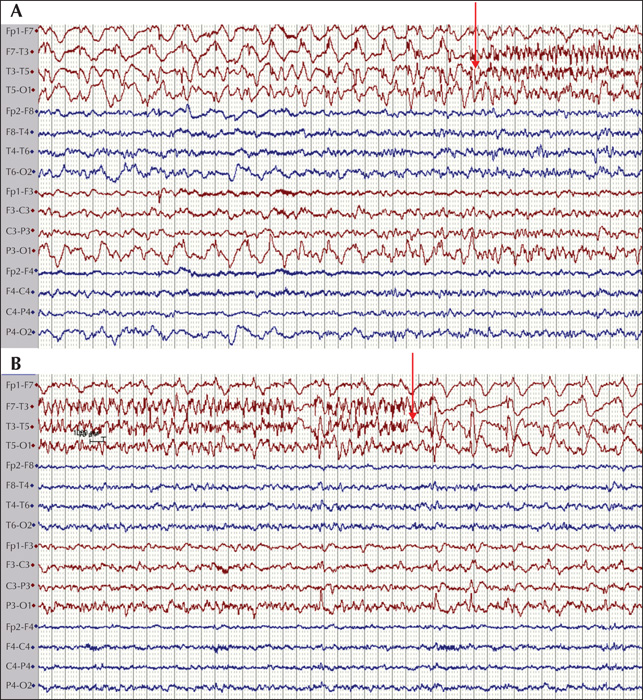
Figure 2
EEG from an 11-month-old female with initial HSV-1 encephalitis, which progressed to NMDA-R-Ab encephalitis. The patient presented with focal seizures with tonic motor components in her upper and lower limb on the right side. Initial EEG showed repeated spiking over the left temporal regions with seizure activity. Start (A) and end (B) of the seizure are marked with red arrows.
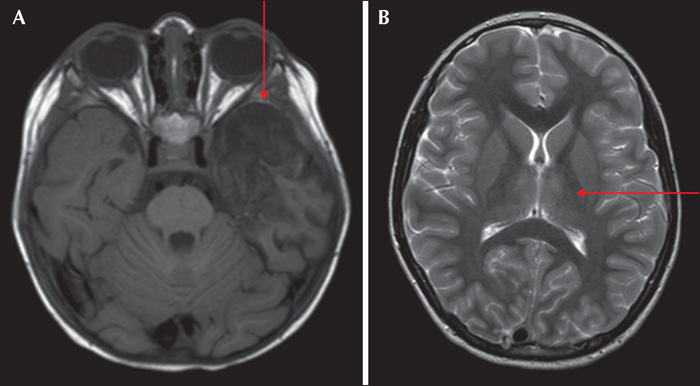
Figure 3
MRI of patients with PEE. (A) An 11-month-old female with initial HSV-1 encephalitis which progressed to NMDA-R-Ab encephalitis. Focal necrosis was seen in the left temporal lobe and insular region (red arrow). This patient had motor seizures involving the left upper and lower limb. (B) A nine-year-old female with Hashimoto's encephalitis with increased T2-signal in the thalamus bilaterally (red arrow). Similar to the bilateral MRI findings, the EEG and clinical seizures did not show any lateralising features.
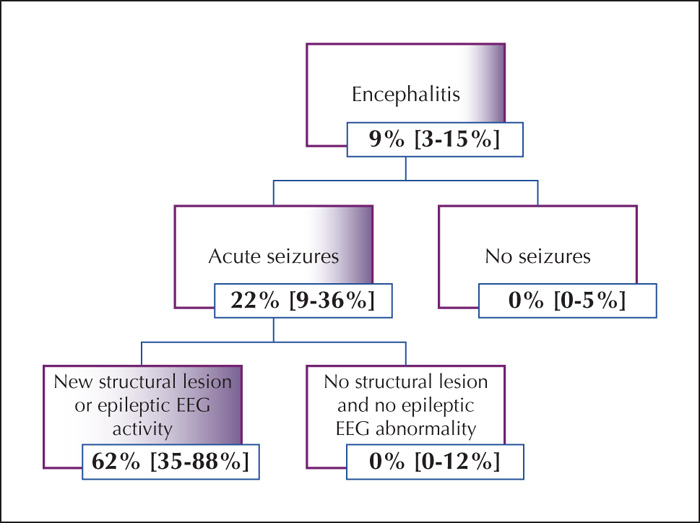
Figure 4
Algorithm for cohorting patients into groups with increased risk of developing post-encephalitic epilepsy. For each group, the risk of developing post-encephalitic epilepsy is noted together with 95% confidence intervals. Note the risk estimated at approximately 60% in the final subgroup which might indicate a group that could benefit from AED treatment.

