Magnesium Research
MENUMagnesium enhances cardiomyocyte proliferation and suppresses cardiac fibrosis induced by chronic ACTH exposure in rats Volume 34, numéro 2, April-May-June 2021
- Mots-clés : adrenocorticotropic hormone, cardiac fibrosis, cardiomyocyte proliferation, magnesium, stress
- DOI : 10.1684/mrh.2021.0484
- Page(s) : 74-83
- Année de parution : 2021
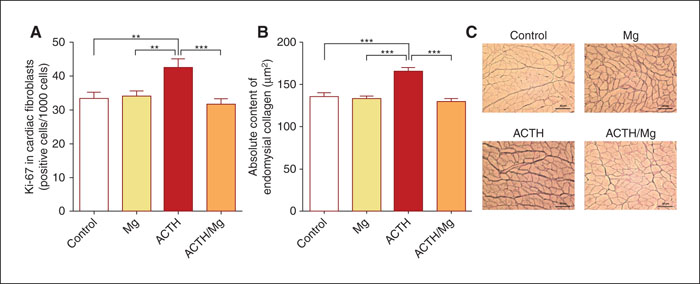
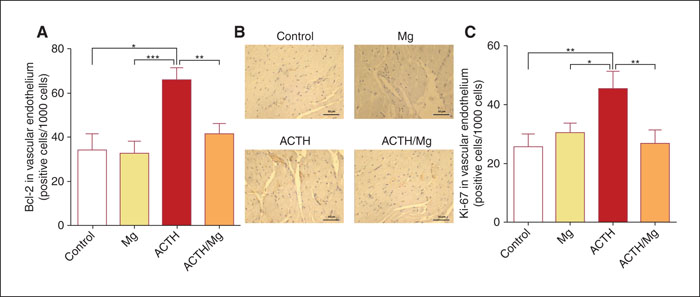
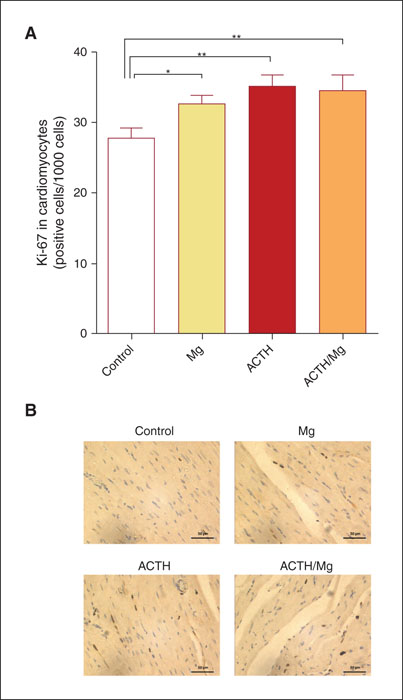
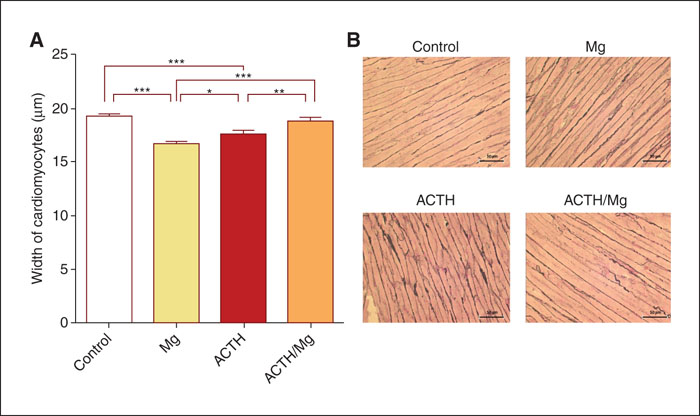
Chronic stress has been implicated in the development and progression of heart disease. In the past decade, a link between chronic stress and cardiac fibrosis has been described. Here, we focused on investigating the effects of one of the key molecular effectors of the stress response–adrenocorticotropic hormone (ACTH) on cardiac histopathology. More importantly, as the literature data support interplay between magnesium (Mg) and the hypothalamo-pituitary-adrenal (HPA) stress system, we explored potential cardioprotective effects of Mg supplementation in a rat model of ACTH-induced cardiac remodeling. Protracted ACTH exposure in rats resulted in a prominent increase in proliferation of fibroblasts and excessive collagen deposition in the heart, accompanied by enhanced proliferation of cardiomyocytes and vascular endothelial cells. Our results show, for the first time, that administration of Mg in rats was effective in ameliorating the development of ACTH-evoked cardiac fibrosis, while facilitating cardiomyocyte proliferation. Furthermore, we propose that Mg supplementation attenuates ACTH-induced HPA axis hyperactivity, as one of the underlying plausible mechanisms, which may contribute to its cardioprotective effects.