Magnesium Research
MENUEffects of perioperative magnesium on postoperative analgesia following thoracic surgery: a meta-analysis of randomised controlled trials Volume 36, numéro 4, December 2023
- Mots-clés : Perioperative magnesium, thoracic surgery, postoperative pain, opioid-sparing effect
- DOI : 10.1684/mrh.2024.0522
- Page(s) : 54-68
- Année de parution : 2023
Objectives
To evaluate the analgesic effects of intravenous magnesium in patients undergoing thoracic surgery.
Methods
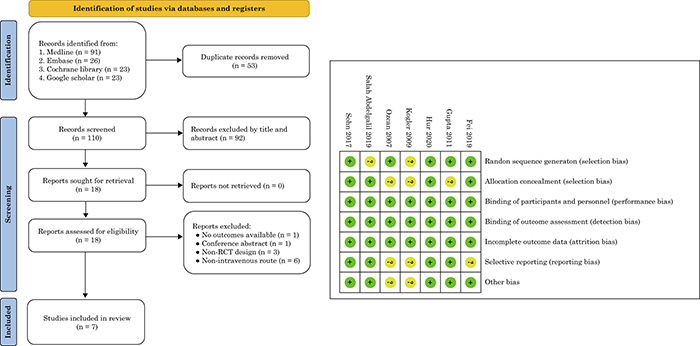
Randomised clinical trials (RCTs) were systematically identified from MEDLINE, EMBASE, Google Scholar and the Cochrane Library from inception to May 1st, 2023. The primary outcome was the effect of intravenous magnesium on the severity of postoperative pain at 24 hours following surgery, while the secondary outcomes included association between intravenous magnesium and pain severity at other time points, morphine consumption, and haemodynamic changes.
Results
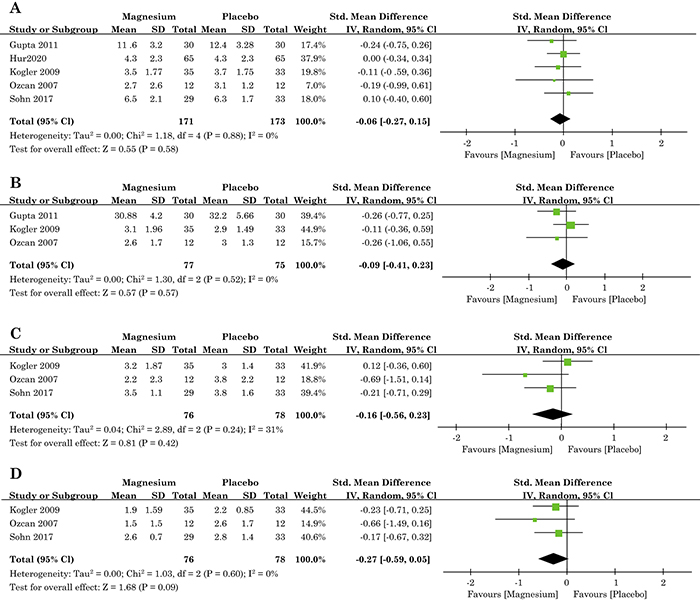
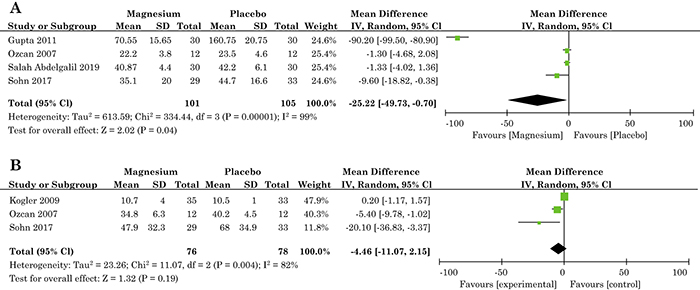
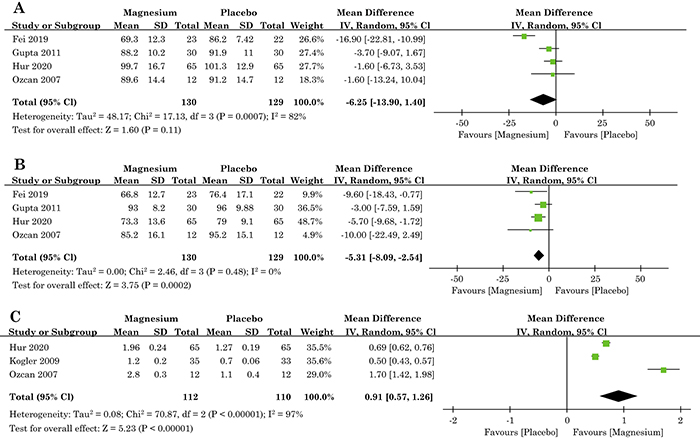
Meta-analysis of seven RCTs published between 2007 and 2019, involving 549 adults, showed no correlation between magnesium and pain scores at 1-4 (standardized mean difference [SMD]=-0.06; p=0.58), 8-12 (SMD=-0.09; p=0.58), 24 (SMD=-0.16; p=0.42), and 48 (SMD=-0.27; p=0.09) hours post-surgery. Perioperative magnesium resulted in lower equivalent morphine consumption at 24 hours post-surgery (mean difference [MD]=-25.22 mg; p=0.04) and no effect at 48 hours (MD=-4.46 mg; p=0.19). Magnesium decreased heart rate (MD = -5.31 beats/min; p=0.0002) after tracheal intubation or after surgery, but had no effect on postoperative blood pressure (MD=-6.25 mmHg; p=0.11). There was a significantly higher concentration of magnesium in the magnesium group compared with that in the placebo group (MD = 0.91 mg/dL; p<0.00001).
Conclusion
This meta-analysis provides evidence supporting perioperative magnesium as an analgesic adjuvant at 24 hours following thoracic surgery, but no opioid-sparing effect at 48 hours post-surgery. The severity of postoperative pain did not significantly differ between any of the postoperative time points, irrespective of magnesium. Further research on perioperative magnesium in various surgical settings is needed.