Epileptic Disorders
MENUStimulus-induced rhythmic, periodic ictal discharges during funduscopic examination in a patient with status epilepticus Volume 21, numéro 5, October 2019
Stimulus-induced rhythmic, periodic, or ictal discharges (SIRPIDs) were described in 2004 (Hirsch et al., 2004) to be consistently induced by alerting stimuli, e.g. auditory stimuli, sternal rubbing, suction, turning, and other nursing interventions in critically-ill encephalopathic patients. A careful clinical-EEG correlation is necessary to recognize these patients. Common causes include hypoxic injury, traumatic brain injury, and haemorrhage, as well as toxic-metabolic disturbances. Here, we report a patient with status epilepticus showing unique SIRPIDs during funduscopic examination, which is worthy of attention.
Case study
A 20-year-old man, without prior seizure history, experienced a week of low-grade fever, nausea, vomiting, and diarrhoea, as a viral infection, in a local clinic, and was prescribed symptom-relieving medications. One week later, sudden onset of bouts of generalized tonic-clonic seizures occurred. His laboratory data during admission, including electrolytes, were essentially normal except for mild elevated creatine kinase and mild leukocytosis, probably related to seizures in clusters. A CT scan of the head was unremarkable. There was no focal sign identified during neurological examination. His cerebrospinal fluid analysis showed leukocytosis with lymphocyte predominance, without glucose consumption. The lactic acid level was normal. His pupils remained with bilateral isocoria and obvious direct light reflex.
Due to impending status epilepticus, for airway protection, he was intubated. Chest X-ray revealed acute pulmonary oedema. His oxygen demand increased and he was paralyzed under non-polarizing muscle relaxant cisatracurium therapy. His first EEG showed intermittent bilateral unsynchronized large delta waves or groups, followed by generalized attenuation, without obvious focal slowing. Follow-up EEG showed episodic prominent generalized spike-and-waves, with progression in duration. Continuous EEG monitoring was then implemented.
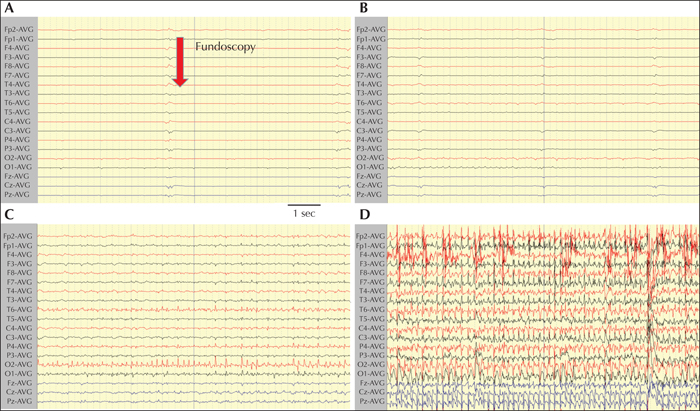
On the second day, an apparent ictal discharge and clinical seizures were frequently noted when performing nursing care. He was administered phenytoin (100 mg every eight hours) and midazolam (0.2 mg/kg/hr). Importantly, during standard funduscopic examination of his left eye, gradually developing fast-frequency spikes, appearing from electrodes T6 and O2, were noted, without clinically overt movement. Twenty-five seconds later, ipsilateral and contralateral hemispheric spreading occurred, which developed into a clinical generalized tonic-clonic seizure (figure 1). The funduscopic examination was discontinued while the seizure occurred. The EEG reaction to funduscopy was longer than the actual duration of the stimulus.
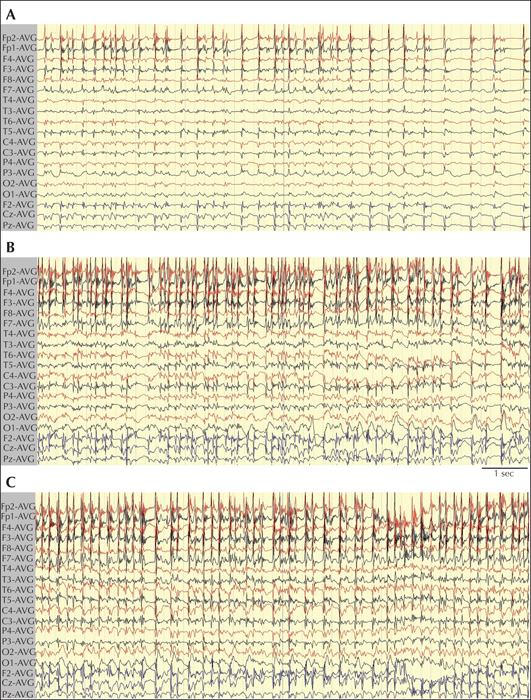
There were also interictal diffuse abnormalities outside of the funduscopic stimulation, mainly quasi-periodic high-amplitude spikes, predominantly in the right frontal area (Fp2F4F8), which intermittently evolved into quasi-periodic generalized spikes, corresponding to a clinical generalized seizure (figure 2).
Owing to refractory status epilepticus, high-dose propofol (10 mg/kg/hr) was administered, in addition to standard antiepileptic drugs. Bradycardia developed on the fourth day and despite high dosage of propofol and extracorporeal membrane oxygenation, this patient expired on the fourth day.
Discussion
SIRPIDs are reported in the literature; most of the stimuli are alerting stimuli with rare exceptions (Hirsch et al., 2004; Lin et al., 2016), including nursing, suction, and noxious stimuli (Lin et al., 2016). We have reported one case in which SIRPIDS were evoked by performing corneal reflex examination (Lin et al., 2016). To our knowledge, this is the first report of development of SIRPIDs during funduscopic examination.
In this case, a certain threshold of light intensity would be required, as there was no SIRPID evoked during simple light reflex examination. The relative strong light from the funduscope stimulated his left eye (cornea), approaching the fundus (retina), then the optic nerve, chiasm, lateral geniculate nuclei, optic radiations and eventually reaching the occipital cortex, and subsequently provoking SIRPIDs, as evidenced by the ictal EEG recording. It is thus possible that the encephalitis in this case altered regional cortical excitability, especially the unilateral (right) occipital cortex. The lack of similar response during funduscopic examination of the right eye suggests that the altered neuronal excitability associated with SIRPIDs is area specific, even in a patient with diffuse encephalopathy.
Many studies have shown visual-induced seizure activity originating from the occipital cortex (Guerrini et al., 1998), and then spreading forward. One study revealed transient cortical hyperexcitability by blindfolding the participants for 48 hours (Pitskel et al., 2007). On funduscopic examination, a higher intensity of light may play an important triggering role. The limitation of this case study is that no photic stimulation test was performed, which might provide further information about the photoparoxysmal response in this encephalopathic brain.
Factors that affect funduscopic examination include the duration of exposure to light, the size of the incident light beam, the intensity of the light, the foci (areas) to be examined, the angle of appropriate position, the dilation of a pupil, and the photochemical damage to the retina (Wolffe, 2016). Further clinical studies are required to address appropriate eye care in the management of patients with potential SIRPIDs during funduscopic examination.
Supplementary data
Summary didactic slides are available on the www.epilepticdisorders.com website.
Acknowledgements and disclosures
This work was supported in part by grants from the Ministry of Science and Technology, Taiwan (107-2314-B-006-018-, 107-2320-B-006-019-, 108-2320-B-006-023-), and the National Cheng Kung University Hospital, Taiwan (20180254, 20190160). This case report was presented at the Taiwan Epilepsy Society Annual Meeting in 2013. The authors would like to give special thanks to Dr. Ilo Elmar Leppik (USA) for comments on this case.
None of the authors have any conflict of interest to declare.