Epileptic Disorders
MENUPentobarbital coma therapy for super-refractory status epilepticus and in-hospital mortality: an observational study Volume 23, numéro 6, December 2021
- Mots-clés : super-refractory status epilepticus, pentobarbital coma therapy, pentobarbital infusion dose, prognosis
- DOI : 10.1684/epd.2021.1333
- Page(s) : 833-42
- Année de parution : 2021
Objective
Treatment of super-refractory status epilepticus (SRSE) is associated with various complications of anaesthetic coma therapy. This study aimed to describe the factors affecting the prognosis, especially in-hospital mortality, of patients receiving pentobarbital coma therapy for the treatment of SRSE.
Methods
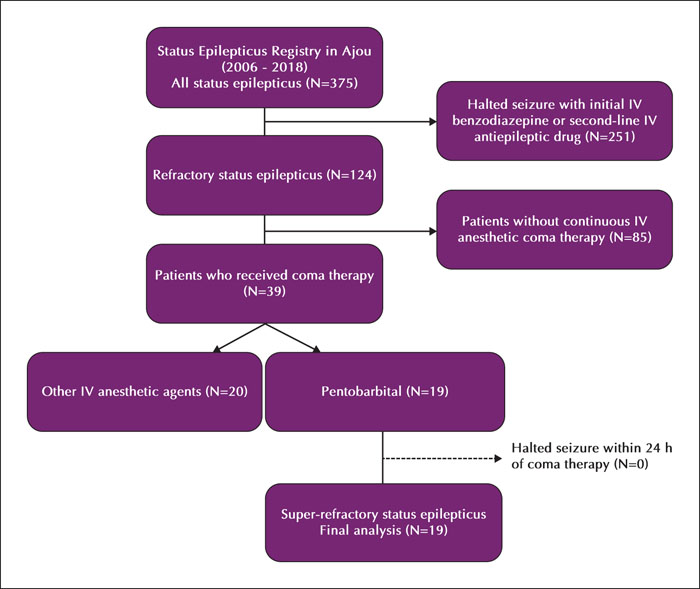
This was a retrospectivecohort study conducted in a single tertiary referral centre with patients who received pentobarbital coma therapy for the treatment of SRSE from 2006 to 2018. Exploratory analyses were performed for clinical, laboratory, electrographic, and radiological factors for the entire cohort and were compared between the mortality and survivor groups.
Results
In total, 19 patients were enrolled, and five (26.3%) patients died in the hospital. The maximal pentobarbital infusion dose was higher in the mortality group than in the survivor group (4.4±1.0 mg/kg/h vs. 2.9±1.4 mg/kg/h, respectively; p=0.025). The high-dose pentobarbital infusion group (>3.75 mg/kg/h) underwent longer mechanical ventilation (24 [20–36.75] vs. 41 [28–70], p=0.025) and blood culture results were more frequently positive, suggestive of septicaemia (8.3% vs. 57.1%, p=0.038).
Significance
The group of SRSE patients treated with pentobarbital coma therapy who died in the hospital received a higher pentobarbital infusion dose compared to survivors; a complication of high-dose pentobarbital infusion was septicaemia. Considering the high rate of septicaemia observed, systematic treatment strategies focusing on infectious complications should be established and implemented. The association between maximal pentobarbital infusion dose and in-hospital mortality needs to be further validated.