Epileptic Disorders
MENUEncephalopathy related to Status Epilepticus during slow Sleep: an historical introduction Volume 21, supplément 1, June 2019
Illustrations
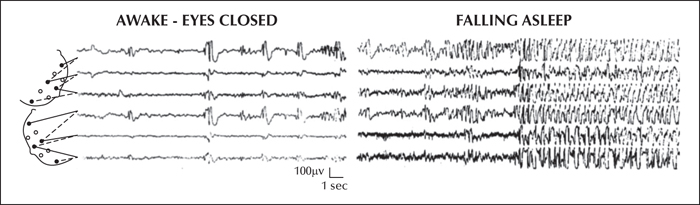
In 1971, Patry, Lyagoubi and Tassinari described in six children a distinctive EEG pattern, referred to as “Subclinical electrical status epilepticus induced by sleep”, characterized by apparently “subclinical” spike-and-wave discharges occurring almost continuously during sleep for a variable length of time (months to years) (figure 1). In 1977, Tassinari et al. reported eleven additional patients. The conclusions of this study (that considered also five of the original patients) stated verbatim: “the sixteen cases exhibit a peculiar electroclinical syndrome for which the term of Encephalopathy related to Status Epilepticus during slow Sleep, or ESES, is suggested. The EEG shows as soon as the subjects fall asleep, continuous high-voltage diffuse slow spike-and-wave discharges which persist throughout the non-REM sleep. During REM sleep the status epilepticus disappears. Status epilepticus during sleep (SES) can persist for years (up to 8 yrs) and it occurs every time the subjects fall asleep. The waking EEG may or may not show various abnormalities: focal, multifocal, diffuse spikes or spikes and waves. The clinical features can be distinguished into three periods: a) Onset: (4 to 8 yrs) with various types of nocturnal (usually rare) and/or diurnal (atypical absences) seizures present in fifteen cases. One subject never had epileptic seizures. b) Status: characterized by a severe psychic syndrome with psychotic behaviour and mental deterioration. The status period spans from 2 to 8 yrs during which every sleep record shows the status epilepticus. c) Remission: in four cases SES disappeared and the subjects showed progressive improvement in behaviour and mental performances. It is suggested that the condition of a protracted (years) SES can be the factor leading to severe mental deterioration and psychic disturbances in some children. In children with rare seizures and appearance of severe psychic and mental impairment, a sleep record should be considered in search of the ESES ”.
As already pointed out (Cantalupo et al., 2013), it is interesting to notice that these conclusions anticipated the concept that was incorporated years later by the International League Against Epilepsy (ILAE) Classification Task Force into the definition of epileptic encephalopathy, including not only the conditions with frequent seizures but also those with a large amount of “interictal” epileptiform activity (Berg et al., 2010).
Kellerman was the first to make the connection between acquired epileptic aphasia, or Landau-Kleffner syndrome (LKS), and extreme activation of spike-and-wave discharges during slow sleep, consistent with SES: “Landau and Kleffner (1957) suggested that persistence of convulsive discharges in the brain tissue concerned with linguistic communication may result in functional ablation of these areas. This assumption is supported by the report of Patry et al. (1971). Four of their six cases with subclinical sleep-induced bioelectrical status epilepticus have total lack or severe delay of speech. Unfortunately in a supplementary report by one of the authors (Tassinari et al., 1977) no further details are given as to whether the additional patients with subclinical status epilepticus showed evidence of aphasia. However, their children suffered from a severe psychotic syndrome and mental deterioration” (Kellerman, 1978).
Indeed, in Tassinari's cases (Tassinari et al., 1977), the language impairement was not the main clinical feature. Most importantly, in the above citation, Landau and Kleffner referred to epileptic activity during wakefulness and not during sleep. In fact, years later, Landau and Kleffner (2009) commented on sleep-related epileptic activity and LKS: “Regarding the epilepsy component of LKS, a major constituent of the syndrome of which we had been unaware, is the tremendous exaggeration of paroxysmal brain activity during sleep. We know that such highly abnormal nocturnal EEG are also associated with other clinical syndromes, suggestive of predominant paroxysmal activity in areas other than the auditory territory ”.
In 1989, the International League Against Epilepsy (ILAE) recognized LKS and ESES (otherwise labelled as epilepsy with continuous spike waves during slow-wave sleep - CSWS) as distinct epilepsy syndromes of childhood (whether focal or generalized) (Commission on Classification and Terminology of the International League Against Epilepsy, 1989). However, since the early 2000s, it became accepted that ESES encompassed LKS, this latter representing a clinical variant or subtype of the former (Tassinari et al., 2000). Indeed, the ILAE Task Force in 2006 acknowledged that the current evidence was insufficient to consider LKS and ESES as separate syndromes (Engel, 2006).
One of the most intriguing issues of ESES is the relationship between SES and the pattern of neuropsychological and/or motor impairment. In recent years, numerous experimental data have shown the crucial role of sleep in physiological cognitive and psychomotor development, particularly during the developmental age. Based on these data, it has been hypothesized that prolonged, sleep-related focal epileptic activity interferes with sleep slow wave activity, particularly at the site of the epileptic focus, hence disrupting the cortical plasticity processes occurring during sleep that are necessary for learning and memory consolidation of what has been acquired in wakefulness, ultimately resulting in neuropsychological and behavioural disorders (Tassinari and Rubboli, 2006). In fact, some recent reports support this hypothesis, by providing electrophysiological evidence that physiological parameters related to NREM slow-wave activity are impaired in children with ESES and recover after ESES resolution (Bölsterli et al., 2011, 2017). These concepts, that provide a fascinating pathophysiological explanation linking the cognitive impairment to the sleep-related exaggerated epileptic activity that characterize ESES, are efficaciously conveyed by the eponym “Penelope syndrome” in which the ‘cognitive threads’ (neuronal networks) that are weaved during the day are unravelled (by continuous “spiking”) during the night (Tassinari et al., 2009).
Disclosures
None of the authors have any conflict of interest to declare.