Epileptic Disorders
MENUEffectiveness of multimodality treatment for autoimmune limbic epilepsy Volume 16, numéro 4, December 2014
- Mots-clés : limbic encephalitis, paraneoplastic syndrome, autoimmune epilepsy, status epilepticus, rituximab
- DOI : 10.1684/epd.2014.0703
- Page(s) : 494-9
- Année de parution : 2014
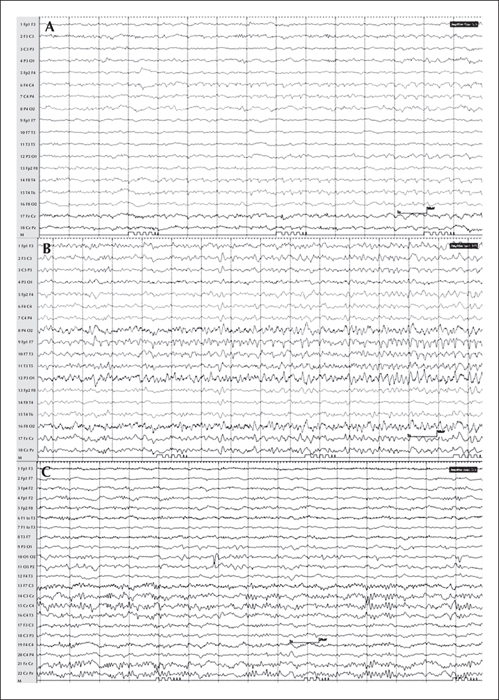
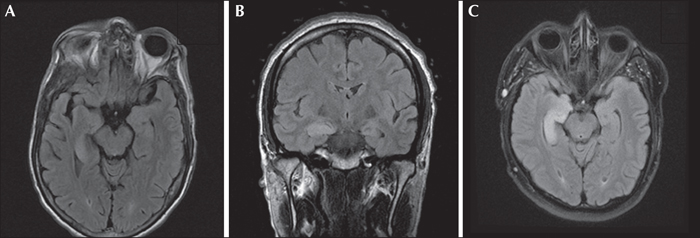
We evaluated the outcome of multimodality treatment in autoimmune limbic epilepsy in 3 consecutive patients (2 male and 1 female; age 33-55 years) presenting with a combination of focal non-convulsive status epilepticus, memory impairment, and psychosis. MRI showed right or bitemporal T2 or FLAIR hyperintensity. Video-EEG showed seizures of right temporo-occipital or bitemporal independent onset. Extensive workup failed to reveal infectious aetiology or an underlying tumour. However, the autoantibody panel was positive for one or more of these antibodies: anti-VGKC, anti-GABAB, anti-VGCC (P/Q, N types), and anti-GAD65. All patients received: (1) conventional antiepileptic drugs including levetiracetam, lacosamide, phenobarbital, lamotrigine, and valproate; (2) immunomodulatory therapy including methylprednisolone, plasmapheresis, and intravenous immunoglobulin; and (3) rituximab. After a 4-6-week in-hospital course, the seizures resolved in all patients but 2 had persistent memory impairment. None had treatment-related complications. At the time of last follow-up, 2-3 months later, 2 patients remained seizure-free while 2 had residual memory impairment. Our findings suggest that multimodality treatment with a combination of conventional AEDs, immunomodulatory therapy, and rituximab is effective and safe in autoimmune limbic epilepsy.