Epileptic Disorders
MENUCochrane systematic review and meta-analysis of the impact of psychological treatment on health-related quality of life in people with epilepsy: an update by the ILAE Psychology Task Force, highlighting methodological changes Volume 23, numéro 6, December 2021
Given the significant impact that epilepsy may have on the health-related quality of life (HRQOL) of individuals with epilepsy and their families, there is increasing interest in evidence-based psychological treatments, aimed at enhancing mental health and seizure-related outcomes for this group. This is a summary of the 2020 update [1] of the 2017 Cochrane Review [2] of controlled studies of psychological treatments in people with epilepsy (PWE). The objective was to assess the impact of psychological treatments on HRQOL outcomes in PWE. The update included major methodological modifications and the latest results.
Methods
Search methods
In this update, we searched the following databases on 12 August 2019, without language restrictions: Cochrane Register of Studies (CRS Web), which includes randomized or quasi-randomized controlled trials from the Specialized Registers of Cochrane Review Groups including Epilepsy, the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (Ovid, 1946 to 09 August 2019), and PsycINFO (EBSCOhost, 1887 onwards), and PubMed, Embase, ClinicalTrials.gov, and the World Health Organization International Clinical Trials Registry Platform (ICTRP). In addition, we screened the references from included studies and relevant reviews.
Selection criteria
We considered randomized controlled trials (RCTs) and quasi-RCTs that investigated psychological treatments for people with epilepsy using HRQOL as a primary or secondary outcome measure. We included a broad range of psychological treatments designed to improve HRQOL, seizure frequency or severity, as well as mental health comorbidities for adults and children with epilepsy. These psychological treatments were variously compared to treatment as usual (TAU, which most commonly included follow up with neurologists or epileptologists for pharmacological treatment of seizures), an active control group (e.g., a social support group with equivalent contact hours), or antidepressant pharmacotherapy (in studies that included patients with epilepsy and comorbid mood disorder).
Re-categorization of psychological interventions
While the previous review had grouped psychological interventions in five groups: psychological interventions, self-management/family management, adherence, (psycho-) educational and mixed interventions, these were collapsed into two categories in this updated Cochrane review: (1) education-only interventions and (2) skills-based psychological interventions. The new operational categorization emphasized commonalities of the interventions’ components rather than differences, and was intended to increase comprehensibility. Education-only interventions were defined as those that provide epilepsy-related facts and knowledge, while skills-based psychological interventions (which may involve educational elements) require an engaged learner who acquires and applies skills and knowledge to achieve psychological and behavioral changes.
Data collection and analysis
We used the standard methodological procedures required by Cochrane [3].
Results
The 2017 Cochrane review included 24 completed RCTs (2,439 participants); this updated review included 36 completed RCTs, with a total of 3,526 participants. The 50% growth in trials in just two years demonstrated the growing interest in the investigation of psychological interventions for people with epilepsy. Of these studies, 27 investigated skills-based psychological interventions [4-30]. The remaining nine studies were education-only interventions [31-39]. Five studies investigated interventions for children and adolescents [24, 30, 35, 36, 39], six for adolescents and adults [12, 20, 29, 31, 32, 34], and the remaining studies for adults only.
Expanded risk of bias assessment in studies of psychological interventions
Due to an increased interest in risk of bias domains in evaluating psychological interventions [40], we considered three additional potential sources of bias in this updated review, including (1) fidelity to the intervention protocol, (2) competence in treatment delivery, and (3) selective recruitment. We contacted authors to gather this additional information.
Features of therapeutic interactions may vary from therapist to therapist, and this may be an inherent characteristic in psychological interventions. Efforts in measuring fidelity to psychological intervention protocols and competence in treatment delivery have been increasingly recognized in recent years [40].
In our included studies, little information was provided to judge risk of bias in terms of fidelity to the intervention protocol. Six studies reported the use of measures to assess fidelity. While two recent studies reported the actual results of their analysis [27, 32], results of the described fidelity assessment of one of the older studies was provided by the authors upon our request [28]. Moreover, three additional studies disclosed details on their procedures to assess fidelity to the intervention protocol [22, 24, 33]. We rated risk of poor fidelity to treatment protocol as ‘low’ in all of these studies. We also considered the risk of poor fidelity to the intervention protocol as ‘low’ in three studies in which the delivery of the intervention was internet-based [10, 26, 41]. All remaining studies were rated as ‘unclear’, in terms of risk of poor fidelity to intervention protocol.
Two dimensions of competence in treatment delivery were assessed. First, we reviewed the competence in terms of the professional training background of personnel who delivered the intervention. Second, we reviewed the competence of the measures used to assess the quality of actual treatment delivery. In internet-based intervention programs, we only evaluated the training background of the professionals who had designed the intervention. Most studies reported the training background of personnel delivering the intervention, and risk of bias was therefore rated ‘low’ in these studies (n = 28 studies). In terms of the quality of actual delivery as a component of competence, four studies reported the use of measures to assess competence and these results were reported in three studies [7, 28, 32]. Three authors provided additional details about their attempts to assess competence with reported results [9, 16, 17]. Consequently, we judged the risk of poor competence to be ‘low’ in all six studies and to be ‘unclear’ for the remaining studies.
Risk of selective recruitment was considered ‘low’ in all 13 studies that reported consecutive recruitment at the intervention site including screening of all patients for eligibility [5, 7, 9, 13, 18, 20, 24, 27-29, 32-34]. Risk of selective recruitment was considered ‘high’ in all studies in which the recruitment procedure involved subjective criteria (n = 2: [4, 22]), advertisements (n = 9: [8, 10, 15-17, 21, 26, 31, 35]) or convenience sampling (n = 1: [6]). Recruitment procedures were ‘unclear’ in all remaining studies.
The risk of bias assessment of all domains is shown in supplementary figure 1. Limited ability to blind participants and personnel in trials investigating psychological interventions continued to be the area for which the risk of bias is highest. Implications for psychotherapy research are discussed below in future directions.
The reception of psychological interventions depends on participants’ motivation to actively engage in the intervention, and attrition across the intervention and follow-up period also continued to be high in more recent trials (see supplementary figure 1).
Characteristics of interventions, designs, and participants included in meta-analysis
Based on satisfactory clinical and methodological homogeneity among the skills-based interventions, we pooled data from 11 studies (643 participants) that used the Quality of Life in Epilepsy-31 (QOLIE-31) or other QOLIE inventories (such as QOLIE-89 or QOLIE-31-P) convertible to QOLIE-31 [4, 8, 9, 11, 12, 14, 18, 20-22, 29]. The control groups comprised treatment as usual (n = 5), waiting-list control (n = 2), antidepressant pharmacotherapy (n = 2), supportive therapy (n = 1), and an alternative psychological intervention (n = 1).
The skills-based interventions that were included in meta-analysis comprised five trials with a main treatment goal of reducing depressive symptoms [8, 9, 11, 12, 14], two self-management interventions [21, 22], two mixed interventions (self-management and memory training, psychoeducation and counseling) [20, 29], one mindfulness-based intervention with a main treatment goal of improving HRQOL [18], and one cognitive-behavioral therapy intervention primarily aimed at reducing seizures [4]. The median duration of the interventions included in the meta-analysis was eight weeks (range: 8 weeks-2 years). The median number of sessions was eight (range: 5 – 20) on a weekly (n = 8), biweekly (n = 2), or an irregular (n = 1) basis. Three interventions included a median of four monthly booster sessions (range: 1 - 9) following the more frequent treatment period [12, 14, 22].
The majority of interventions were delivered in a group format (n = 6= [4, 11, 12, 18, 21, 22]. In the remaining five trials, interventions were delivered in an individual format; two of these trials included an initial psychoeducation session in a group format [20, 29]. Individual sessions lasted between 50 minutes and one hour, while group sessions lasted between one hour and 2.5 hours. The duration of sessions was unknown in two trials [12, 20]. The interventions were delivered by psychologists (n = 6), epilepsy nurses (n = 4), social workers (n = 2), licensed therapists (n = 1), and a psychiatrist (n = 1). Two group interventions were delivered by interprofessional teams [11, 12] and two involved peer mentors [21, 22]. Intervention delivery in five trials had been manualized [8, 12, 14, 21, 29]; in two of these trials, interventionists (social workers, nurses) had received two days of training prior to the delivery of the intervention manuals [14, 29] (see table 1). Two of the 11 meta-analyzed studies included adolescents only [12] or adults and adolescents [29], respectively. All other studies included only adults; none of the studies in the meta-analysis included children. The exact percentage of all study participants (n=675) who had drug-resistant epilepsy and depression could not be calculated based on the information provided, e.g. some trials did not capture whether patients had a depressive episode at baseline. However, at least 53% (353 participants) were not seizure-free and at least 35% (234 participants) were likely to be clinically depressed based on a structured clinical interview (98 participants), scores on self-report questionnaires (94 participants) or prescription of antidepressants (42 participants) at the time of recruitment.
Meta-analysis
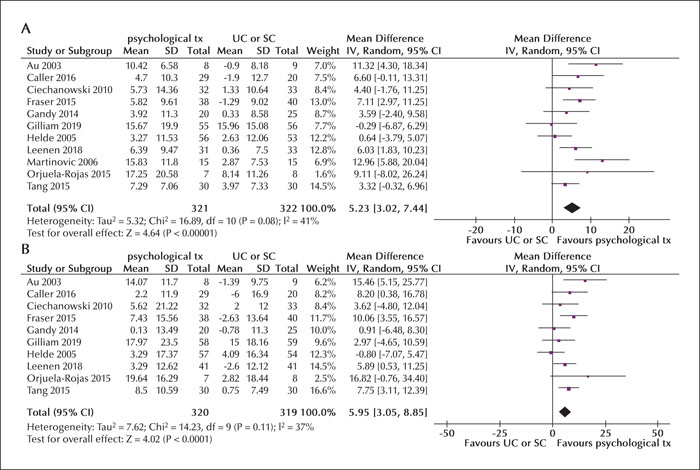
As in the previous review, we found significant mean changes in the QOLIE-31 total score and in six out of seven subscales (emotional well-being, energy and fatigue, overall QoL, seizure worry, medication effects, and cognitive functioning). The mean changes in the QOLIE-31 total score (mean improvement of 5.23 points, 95% CI: 3.02 to 7.44; p < 0.001), and the overall QoL score (mean improvement of 5.95 points, 95% CI: 3.05 to 8.85; p < 0.001) exceeded the threshold of minimally important change (MIC: QOLIE-31 total score: 4.73 points; overall QoL score: 5.22 points), indicating a clinically meaningful post-intervention improvement in HRQOL (see figures 1A, B) [42].
In the previous Cochrane review [2], the total score and three subscales (emotional well-being, energy and fatigue, and overall QOL) had exceeded the minimally important change (MIC) threshold. However, in this update, we downgraded the certainty of the evidence provided by the initial meta-analysis due to serious risks of bias uncovered in some of the included studies (see supplementary figure 1). Consequently, these results are now judged to provide evidence of moderate certainty that psychological treatments for adults with epilepsy may enhance overall HRQOL.
Conclusions
Implications for clinical practice
Skills-based psychological interventions improve HRQOL in adults and adolescents with epilepsy. Adjunctive use of skills-based psychological treatments for adults and adolescents with epilepsy may provide additional benefits in HRQOL when incorporated into patient-centered epilepsy management. We judge the existing evidence to be of moderate certainty. Practical conclusions for education-only interventions have previously been formulated in a separate evidence-based recommendation paper by the ILAE Psychology Task Force [43]. The use of psychological interventions is another resource in the armamentarium for management of PWE.
Implications for research design and reporting
Based on the 2017 Cochrane review [2], recommendations for the implementation of psychological clinical trials in epilepsy have been formulated [44]. Investigators are encouraged to strictly adhere to the CONSORT guidelines in order to improve the quality of reporting of their psychological interventions. A thorough description of intervention protocols is necessary to ensure reproducibility. When examining the effectiveness of psychological treatments for people with epilepsy, the use of standardized HRQOL inventories, such as the Quality of Life in Epilepsy Inventories (QOLIE-31, QOLIE-31-P, and QOLIE-89) would increase comparability. In order to increase the overall quality of RCT study designs, adequate randomization with allocation concealment and blinded outcome assessment should be pursued, where feasible. As attrition is often high in clinical trials that require active participation, an intention-to-treat analysis should be carried out. In order for RCTs in this area to inform clinical practice with greater confidence, attention should be paid to the assessment of treatment fidelity and treatment competence. Lastly, given that a clinician cannot be blinded to what type of therapy they are giving, and that a patient/participant will also know that they are receiving a particular therapy, conducting a “double-blind” psychotherapy trial is not possible. In light of that design impossibility for psychotherapy trials, the risk bias rating for the intervention masking could be mitigated by including outcome raters who are blinded to which arm the participant is enrolled. Future high-quality studies of psychological interventions for PWE may provide support for these and other interventions.
Depression has a strong association with HRQOL in epilepsy, and psychological interventions (particularly cognitive behavioral therapy) are recognized as effective therapies for depression. Hence, future studies of psychological interventions should include a sub-analysis of patients with major depression and delineate to what extent improvements in HRQOL in epilepsy are mediated by the reduction of depressive symptoms.
Identified gaps and future directions
With increasing evidence that psychological treatments benefit adults and adolescents with PWE, there has been much discussion on resource allocation informed by the identification of care priorities. Participants in our included studies were heterogeneous regarding seizure control, drug responsiveness and psychiatric comorbidities. Some studies did not include these characteristics as criteria for patient selection, while some delivered psychological treatment to a specific group of patients with epilepsy (e.g. drug-resistant epilepsy, epilepsy and comorbid depression). We recommend that psychological treatments be incorporated as part of standard comprehensive care for PWE. However, with a reasonable concern for limited resources, future studies with subgroup analyses (e.g. drug-resistant epilepsy, epilepsy with distinct comorbid psychiatric disorders) and health economic outcome measures (e.g. direct and indirect health care costs; common metrics used in cost-effectiveness analyses: cost per quality-adjusted life year [QALY] gained and cost per disability-adjusted life year [DALY]) may provide further insights into optimal resource allocation.
Of note, only a small number of RCTs were conducted on pediatric populations. A similar gap has been identified in trials on PWE and comorbid intellectual disabilities, including special training for their caregivers. Further development on psychological treatment protocols specifically for these populations is needed.
Supplementary material
Supplementary figure and summary slides accompanying the manuscript are available at www.epilepticdisorders.com.
Acknowledgements and disclosures
RM received funding from the internal grant program (project IFF 2020-28) of the Faculty of Health at Witten/Herdecke University, Germany. MG is supported by a Macquarie University Research Fellowship. This paper describes independent research, partly funded (LHG) by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King's College London. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. KV received funding from the National Council for Scientific and Technological Development (307817/2019-9)
This report was written by experts selected by the International League Against Epilepsy and was approved for publication by the ILAE. Opinions expressed by the authors, however, do not necessarily represent the policy or position of the ILAE. The authors report no disclosures. This publication represents work of the ILAE Psychology Task Force members. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
* This article is based on a Cochrane Review published in the Cochrane Database of Systematic Reviews (CDSR) 2020, Issue 8: CD012081. DOI: 10.1002/14651858.CD012081.pub3 (see www.cochranelibrary.com for information). Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, and the CDSR should be consulted for the most recent version of the review.