Epileptic Disorders
MENUExternal validation of the Epilepsy Surgery Grading Scale in a Japanese cohort of patients with epilepsy Volume 23, numéro 1, February 2021
- Mots-clés : epilepsy surgery, grading scale, validation study
- DOI : 10.1684/epd.2021.1238
- Page(s) : 104-10
- Année de parution : 2021
Objective
The Epilepsy Surgery Grading Scale (ESGS) is a simple method to predict the likelihood of a patient with epilepsy proceeding to surgery and achieving seizure freedom. Usefulness of the ESGS has been confirmed in established epilepsy centres in the United States and Belgium for adult patients with drug-resistant focal epilepsy undergoing presurgical evaluation. However, the applicability of the ESGS has not yet been evaluated in a wider range of epilepsy patients that may reflect the general spectrum of epilepsy. The present study validated the ESGS in a Japanese epilepsy centre in which admission-based comprehensive epilepsy studies were indicated beyond presurgical evaluation.
Methods
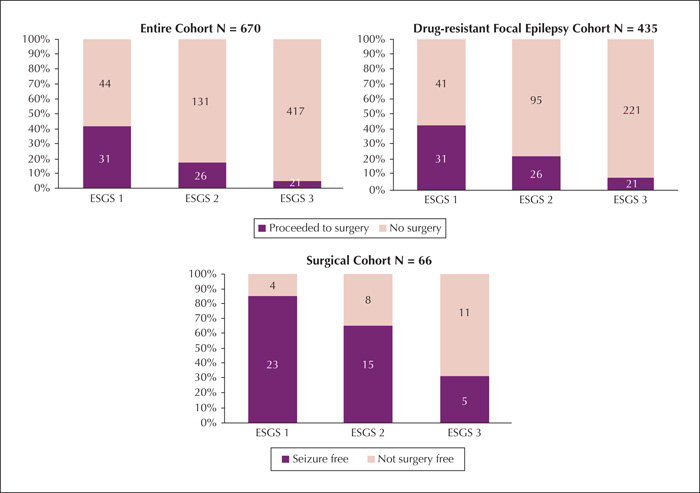
This single-centre retrospective study included adult patients with epilepsy admitted to the Epilepsy Monitoring Unit from 2010 to June 2019. Patients were classified as ESGS Grade 1 (most favorable), Grade 2 (intermediate), and Grade 3 (least favourable). Patients were grouped into three cohorts: all patients, patients with drug-resistant focal epilepsy, and patients who underwent resective epilepsy surgery. We assessed progression to surgery and seizure freedom at one year after surgery.
Results
Of the 1,158 total admissions, 670 patients met the inclusion criteria and formed the total cohort. Of these, 435 (64.9%) had drug-resistant focal epilepsy and 78 (11.6%) proceeded to resective surgery. Overall, progression to surgery was observed in 41.3%, 16.6%, and 4.8% of patients with Grade 1, 2, and 3, respectively. In the surgical cohort, seizure freedom was observed in 85.2%, 65.2%, and 31.3% of patients with Grade 1, 2, and 3, respectively.
Significance
Our results indicate that the ESGS is effective in predicting whether a patient proceeds to epilepsy surgery and achieves seizure freedom even in the general population of epilepsy patients, regardless of type or resistance to antiepileptic drugs.