Epileptic Disorders
MENUEvolution of concepts in epilepsy surgery Volume 21, numéro 5, October 2019
Illustrations
Tableaux
- Mots-clés : history, epilepsy surgery, ILAE, EEG, neuroimaging, neuropsychological testing
- DOI : 10.1684/epd.2019.1091
- Page(s) : 391-409
- Année de parution : 2019

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License
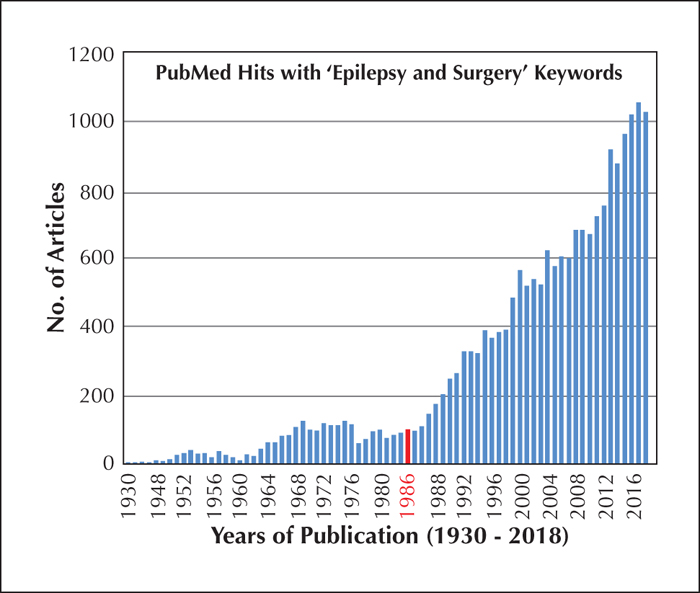
At the time of the first meeting of the International League Against Epilepsy (ILAE) in 1909, surgical treatment for epilepsy had been accepted as an alternative therapy for over two decades, but was rarely practiced, considered a last resort for carefully selected patients. Localization was based on ictal semiology and identification of a structural lesion. Very few papers on epilepsy surgery were presented at ILAE meetings or published in Epilepsia during the first half of the 20th century. A modest explosion in interest in epilepsy surgery at mid-century resulted from recognition that “invisible” epileptogenic lesions could be identified by EEG, especially for temporal lobe epilepsy. Epilepsy surgery received a second boost in popularity toward the end of the 20th century with the advent of structural and functional neuroimaging, and the number of epilepsy centers worldwide doubled between the first Palm Desert conference in 1986 and the second Palm Desert conference in 1992. Neuroimaging also helped to increase application of surgical treatment to infants and young children with severe epilepsies. Epilepsy surgery was accepted as standard of care for drug-resistant focal epilepsy and was well-represented at international ILAE congresses and in Epilepsia. Advances continue into the 21st century with the introduction of laser ablation, and palliative neuromodulation approaches, which have greatly increased the population of patients who can benefit from surgery. Modern presurgical evaluationtechniques have also made surgical treatment possible in many countries with limited resources. Three randomized control trials now have definitively proved the safety and efficacy of epilepsy surgery, however, this alternative therapy remains under-utilized even in the industrialized world, where less than 1% of potential candidates are being referred to epilepsy centers. Furthermore, those who are referred receive surgery an average of 20 years after onset of epilepsy, often too late to avoid irreversible disability. The major challenges in realizing the full potential of epilepsy surgery, therefore, are not as much in the continued improvement of the treatment itself, as they are in addressing the treatment gap that is preventing appropriate patients from being referred to full-service epilepsy centers.