Epileptic Disorders
MENUAtypical presentation of sunflower epilepsy featuring an EEG pattern of continuous spike waves during slow-wave sleep Volume 23, numéro 6, December 2021
Sunflower epilepsy (SE) is a rare photosensitive epilepsy characterized by stereotyped hand waving coupled with generalized 3-4-Hz spike-and-wave discharges on EEG [1, 2]. Patients with SE stare at a light source, most commonly the sun, and wave their abducted fingers in front of their eyes. Seizure semiology may include eyelid myoclonia with or without absence seizures, myoclonic jerks, and generalized tonic-clonic seizures, whereas the latter may relate to prolonged hand waving episodes [1, 3]. Although the original description suggested that hand waving episodes may induce seizure activity [4], this view is inconsistent throughout the literature. Two recent case series suggested that hand waving is part of the ictal semiology and not a precipitating factor for epileptic seizures [1, 5]. The latter hypothesis also draws from the varying relationship between the hand waving episodes and the associated generalized EEG abnormalities in these patients [6]. Previous reports have supported a female predominance with epilepsy manifestation during the first decade and a significantly higher rate of positive family history for epilepsy than in other photosensitive epilepsies. In contrast to other photosensitive epilepsies, SE is refractory to anti-seizure drug treatment that rarely attains lasting seizure freedom [1, 2, 7]. In line with the poor treatment response, high rates of cognitive deficit of up to 50% have been reported in older case series, particularly in patients with early seizure onset [8]. In contrast, recent cohorts include a majority of children with normal cognitive functions , albeit with occasional attention deficit, speech, language and gross motor deficit, and academic difficulties [1, 2].
Case study
A nine-year-old girl was referred to us due to stereotyped recurrent episodes of staring at the sunlight while performing waving movements with one or the other hand in front of her face for the duration of a few seconds. These episodes first occurred at the age of eight years without any identifiable triggers such as illness or psychological issues in the family. These episodes, initially perceived as a tic disorder, had occurred up to 50 times on sunny days in the past year, but once also looking into intense artificial light and once while diving into water reflecting sunlight. The patient sometimes presented with eye rolling or fluttering during the episodes and was in a trance-like state, once abruptly stopping at a pedestrian crossing. Immediately after the episodes, she stroked her forehead with her hand as if she wanted to brush an imaginary strand of hair from her face and had retrograde amnesia for the episode.
Interestingly, during the disease, the girl performed stereotyped pirouettes before each hand waving episode, accompanied by loss of consciousness. These pirouettes appeared to be executed involuntarily, driven by the sun, with a rapid rotation of the head towards sunlight (see video sequence). The patient could not hide her attraction to the sun from her family and peers, and the seizure semiology was not affected by their presence. Her personal history and family history were unremarkable. The girl presented with normal motor and cognitive development but developed anxiety and depressive symptoms due to teasing and bullying at school, triggered by episodes of hand waving while attending classes, and thus required psychological support.
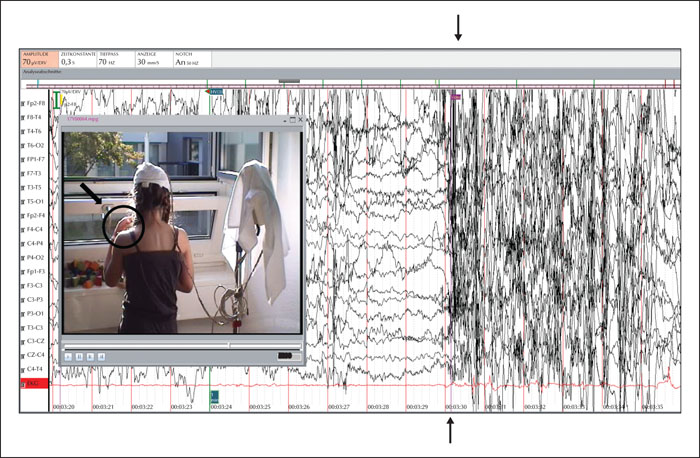
The EEG at initial presentation showed generalized spike-/polyspike-and-wave discharges with frequencies ranging from 1 to 3 Hz and bi-frontal predominance. Hyperventilation led to the activation of the epileptic discharges. Photic stimulation triggered a photo paroxysmal response at 5-20 Hz (figure 1A, B) with brief absences and mild oro-alimentary automatisms in the absence of hand waving, whereas polarized sunglasses diminished this response. The EEG during wakefulness otherwise showed normal background activity (figure 1C). The clinical-neurological examination and brain MRI were normal. The patient was started on levetiracetam (28 mg/kg/day) that showed only a modest effect on seizure frequency, as attested by the parents, and could not be increased because of irritability. At that time, in the hospital setting, staring at the sun alone did not trigger any seizures, despite the frequent epileptic discharges on EEG, whereas the addition of hyperventilation provoked hand waving and an absence seizure (figure 2). It should be noted that, on the same day, the attacks occurred several times outside of the hospital setting.
The first sleep EEG of the patient shortly after diagnosis but before anti-seizure drug treatment fulfilled the criteria of continuous spike waves during slow-wave sleep (CSWS) regarding the EEG pattern (figure 1D), albeit in the absence of neurocognitive regression and behavioural issues and therefore not compatible with CSWS syndrome. CSWS in our patient was defined by a spike-wave index (SWI) exceeding 85% of NREM sleep [9-11] during an overnight sleep EEG recording featuring generalized spike waves with bifrontal and central predominance. Levetiracetam was soon replaced by lamotrigine, and later by add-on ethosuximide. Seizure freedom, including all manifestations of sunflower epilepsy, was eventually achieved under lamotrigine at 8 mg/kg/day and ethosuximide at 27 mg/kg/day, whereas photosensitivity persisted on EEG. Teasing and bullying at school stopped with seizure control. However, an attempt to withdraw anti-seizure medication two years later led to seizure recurrence, including hand waving episodes, which in turn led to a swift increase back up to the initial dosage, again leading to seizure freedom up to the present time. The last neuropsychological evaluation, almost four years after seizure onset, confirmed normal cognition.
Discussion
The chronological sequence of events based on the video-EEG-documented episode of our patient does not appear to support self-induction, at least for this particular episode. Seizure onset on EEG occurred after hyperventilating and while staring at the sun, but before performing the stereotyped hand waving movements that may have produced a flicker effect. On the other hand, blinking itself may also be sufficient to induce seizures, and hand waving is accompanied by blinking in many cases. Ever since the first report by Gastaut in 1951 [4] of two children with photosensitive epilepsy who “appeared to seek a source of light” and then perform repetitive hand waving and head rocking while facing the light, patients with SE have been alleged to deliberately produce flickering and thus self-induce absence seizures. Hand waving and blinking have often been considered to be consistently associated with SE, and therefore difficult to stop. In particular, Gastaut drew attention to the disparity of the light-seeking behaviour in this subgroup of patients [4] and the avoidance of light by other patients with photosensitive epilepsies. However, later case series have supported that hand waving may correspond to an integral part of the epileptic seizure and not to a precipitating factor [12-15]. This controversy was addressed in a recent study that analysed 126 hand waving episodes [5], showing a latency of <1 second between the hand waving and the occurrence of the ictal pattern on EEG, thus suggesting that hand waving itself does not induce seizure activity. Also, it has been previously noted that the photo paroxysmal response on EEG recordings of SE patients commonly occurs at flicker frequencies of 11-14 Hz that are virtually unattainable through voluntary hand waving [16], thus calling into doubt the hypothesis of “self-induced” epileptic seizures. It should be noted that our patient could at least partially suppress the seizures in the hospital setting, thus adding to this controversy. Nonetheless, our case serves to open the discussion on the “self-induction” of epileptic seizures in sunflower epilepsy rather than offer a solution to the riddle surrounding this issue.
Sleep EEG in our patient fulfilled the criteria of a CSWS EEG pattern shortly after SE diagnosis, albeit in the absence of neurocognitive regression. This is the first report of a CSWS EEG pattern in SE that resolved under treatment with ethosuximide and lamotrigine. As in classic absence epilepsy, EEG recordings of SE are commonly performed during wakefulness in order to allow for the application of activating procedures, such as hyperventilation and photic stimulation. The EEG in wakefulness is characterized by generalized epileptiform activity, including 1-4-Hz spike and polyspike wave discharges with frontal or occipital predominance on normal background [1, 2, 12, 13, 17]. This is the first report of a CSWS EEG pattern in SE and is particularly intriguing in comparison to Jeavons syndrome which is otherwise very similar to SE in terms of seizure semiology, interictal and ictal EEG findings, age at onset, female predominance, photosensitivity, and poor response to anti-seizure drugs [6]. In Jeavons syndrome, epileptic discharges on sleep EEG are considerably shorter (and not linked to any clinical manifestation), whereas EEG findings worsen after awakening (and are linked to the occurrence of absences with eyelid myoclonia) [3]. Although we only observed an EEG pattern suggestive of CSWS in the absence of cognitive deficit or deterioration, our case leaves room for speculation on the origin of cognitive deficit in some previously reported cases of SE [1, 2]. While the relationship between the excessive number of epileptic discharges during sleep and the cognitive and behavioural deterioration in CSWS syndrome remains poorly understood, a possible explanation may lie in the impairment of synaptic homeostasis during normal sleep that is particularly crucial for the developing brain [18]. We suggest performing sleep EEG recordings for sunflower epilepsy, particularly in patients with developmental stagnation or regression, in order to avoid overlooking CSWS syndrome that should be timely diagnosed and treated. Our case stresses the importance of sleep EEG recordings even in cases with EEG abnormalities and epileptic seizures during wakefulness.
Seizure freedom, rarely achieved in sunflower epilepsy, has been reached under a combination of ethosuximide and lamotrigine in our patient, while both anti-seizure drugs were well-tolerated at average to high dosages. An attempt to wean anti-seizure drugs after long-term seizure freedom was, however, unsuccessful, and treatment has been reinstalled and continued to date. The mild, treatment-responsive course of the disease in our patient stands in stark contrast to previous reports of a severe, pharmacoresistant course in the majority of patients with SE [1, 2]. In the so far most extensive SE study, including 24 children, adolescents, and young adults, only three patients had a reduction of light-induced seizures under treatment, and none became seizure-free [1]. Broad-spectrum anti-seizure drugs, such as levetiracetam and valproic acid, only proved effective in a minority of patients. Ethosuximide, lamotrigine, and benzodiazepines have also proven effective in eliminating the photo paroxysmal response on EEG and stopping seizures in photosensitive epilepsies [6], but their efficacy in SE has been so far limited. In particular, ethosuximide led to seizure improvement in only one of five children and lamotrigine in only one of seven children in a recent study [2]. In contrast, all nine children treated with valproate had a clinical benefit at relatively low doses, adding to previous studies that support its utilization as first-line treatment for SE [2]. Drawing from our observations, treatment with ethosuximide and lamotrigine may offer an alternative to valproic acid, particularly for girls and young women of childbearing age, for whom valproic acid is contra-indicated. Interestingly, the combination of these two anti-seizure drugs led to the resolution of CSWS in addition to controlling absence seizures.
Paediatric neurologists and epileptologists should be aware of this condition and understand that the hand waving episodes are not necessarily intended to “self-induce” seizures. This approach could help to avoid potential aggravation of the psychological burden and stigma of the disease.
Acknowledgements and disclosures
We thank the patient and her family for sharing their medical history with us and allowing us to publish their data, including the home video. We are very grateful to our EEG technicians, Christine Erne and Cinzia Marcella, for their support.
The authors have no conflicts of interest to disclose.