Journal de Pharmacie Clinique
MENUEvaluation de l’intégration de pharmacien clinicien dans un service de chirurgie orthopédique en France Volume 39, numéro 3, Septembre 2020
Medication errors are defined as any avertable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient and consumer [1]. These errors, preventable in many cases, can occur at any step of the patient path, from prescribing to administration, and take place at home or during hospitalisation.
In France, the number of serious adverse drug events happening during or just after hospitalisation is estimated to be between 275 000 and 395 000 every year, and one in two is a medication error [2]. These errors lead to emergency department visits, with a risk of re-hospitalisation increased to 6 times within 3 months [3], especially in surgery units in which more medication errors occur compared to other disciplines [4]. As a matter of fact, it is known that patients undergoing surgery are commonly victims of medication errors that include errors when entering the hospital, errors during surgery and anaesthesia, errors when transfers and finally errors at discharge [5].
The error rate increases when health care professionals are inexperienced, inattentive, rushed, distracted, tired, or depressed [6]. Also, surgery unit staff may be more likely than others to make medication errors [2]. Surgery is a field which implicates many different professionals, mostly involved in the surgical act. The pathway of an operated patient is complex, consisting of passage through different units (anaesthesia department, intensive care, operating room, conventional care unit…).
One of the solutions proposed to improve medical care by reducing medication errors is the incorporation of pharmacists in medical units. Many studies showed the benefits of clinical pharmacists at various levels: appropriate use of polypharmacy [7, 8], diabetes management [9] or even in medication adherence [10]. Their actions have major clinical [11] and economic impacts [12, 13], particularly in surgery wards [14-17].
In our hospital, a clinical pharmaceutical team (CPT) was implemented into the orthopaedic surgery unit. The CPT carries out medication reconciliation and medication review, optimises therapeutics and is involved in setting the antibiotherapy policy. The medication reconciliation aims at preventing or correcting treatment errors occurring during patient hospitalisation. This is done by obtaining an exhaustive list of all the drugs either taken or to be taken chronically before being hospitalised, prescribed by the doctor or taken as self-medication. Moreover, the CPT produces interventions during the entire hospitalisation for the optimal prescribing. Therefore the clinical pharmacist plays a key role, together with the prescriber.
The objective of this study is to evaluate the proportion of an orthopaedic surgery unit patients processed by the CPT during their hospitalisation, and the acceptance rate of the pharmaceutical interventions. Second objectives are the measuring of the impact on medications errors and on healthcare team satisfaction.
Methods
The clinical pharmacy team development
The orthopaedic surgery unit in which we made this study contained 84 beds distributed throughout three sub-units. The CPT was deployed in it in October 2015. The CPT consisted of a full-time senior pharmacist, supported by a pharmacy resident and two part-time pharmacy students. The CPT was present five days a week, from monday to friday.
The CPT set up a medication reconciliation activity for patients meant to stay more than 24h in the orthopaedic unit. This organisation was decided following the board of directors’ consent and an information meeting with the department staff. The theoretical hospital stays were calculated by the institution, using the surgical indication and the autonomy of the patient.
The pharmacist created an exhaustive medication list by gathering patient data from at least three sources of information. These could originate from medical records, general practitioner, community pharmacy, prescriptions and medicines carried by the patient, district nurse, patient family or computerised pharmaceutical files. This list was the Medication Reconciliation Form, written and computerised by the pharmacist. It was accessible immediately to all hospital staff on the patient's computerized record. The gathered information consisted of patient's data (weight and body mass index, renal function, reason of hospitalisation, medical history, allergies, intolerances, recent antibiotherapy), patient's caregivers details (name of general practitioner, specialists, and usual community pharmacy), and their medicines (name, strength, administration route, dosage and duration). Other types of information were also gathered: treatment adherence, swallowing difficulties or even self-medication.
Medication reconciliation was proactive, i.e carried out before the first hospital prescription if patient was scheduled, or retrospective, if done after the first hospital prescription when patient was not planned. The prescribing physician was contacted every time there were either differences between the Medication Reconciliation Form and the hospital prescription, or new information that was included in them. At the end of a meeting with the prescriber, these divergences were justified or not. If the latter case occurred and the doctor was absent, depending on the severity of the situation, a telephone call was done or a message was written and the medical decision was monitored.
According to the French Society of Clinical Pharmacy (FSCP) classification, pharmaceutical interventions were carried out in case of unintended medication discrepancies between orthopaedic and ambulatory or other hospital prescriptions. An intervention could be classified as non-treated condition, underdose, overdose, not needed medicine, non-conformity with recommendations, inappropriate route or administration, interaction, adverse effects, or lack of monitoring. Two criteria (absence of dosage and absence of strength) were added to be more specific.
In parallel with this activity, the CPT contributed to the therapeutic optimisation in closely monitoring treatments during hospitalisation, in actively participating in multidisciplinary meetings concerning infected patients, or even in giving advice to discharged patients. The prescriptions were analyzed throughout the hospitalization. Optimization proposals were made by the CPT. In these cases, pharmaceutical interventions were also counted.
Evaluation of the impact of the pharmaceutical team
A prospective observational study was made in October 2016, a year after the introduction of the CPT in the orthopaedic surgery unit. This study evaluates their impact on the unit.
Different evaluation criteria were used:
- –The proportion of patients admitted to the hospital who were processed by the CPT over one year. Demographic characteristics of these patients were measured and statistics about their drug consumption were compiled if need be.
- –The number of pharmaceutical interventions made by the pharmacists, and the physicians acceptance rate of these interventions. For each medication to be corrected, an intervention was counted. They were recorded daily to assess their nature, their future (acceptance or refusal of the prescription modifications by medical staff) and if they were performed during the medication reconciliation or during a prescription analyse throughout the hospitalization. Medication errors potential severity was evaluated using the French National Authority for Health method [18] by a pharmacist and a doctor not implicated in the interventions. It was characterized using an algorithm that took into account the nature of the error, the drug's belonging to a list of high-risk drugs, and the clinical, biological and therapeutic context of the patient. They were considered as severe errors whenever they led to an increase in patient monitoring (significant error) at least, to an extension of hospital stay or a reversible (major) or irreversible (critical) impairment, or even play the vital prognosis to cause death (catastrophic).
- –The number of medication errors reported. Medication errors occurring in the surgery unit were freely declared by the nursing staff using a computerised form. After the implementation of the CPT, medication errors could also be declared by the pharmacists. They were recorded by a quality engineer for 10 months before and after the introduction of the CPT. Criticality of the errors was determined by a multidisciplinary group composed of pharmacists, doctors, nurses and quality engineers. It was graduated from low, moderate, high or extreme, by taking into account the severity and the probability of occurrence of the medication errors.
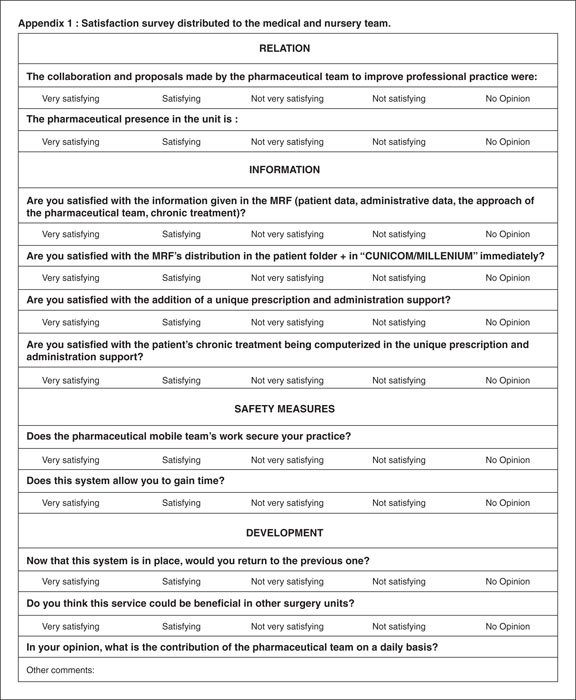
- –The nursing and medical staff satisfaction concerning the CPT. A questionnaire was carried out to assess the satisfaction. It was validated by a quality engineer. Ten questions were asked via Sphinx®, the institutional online software, for the surgical and medical staff or via a paper form for the nursing staff who did not have access to a professional mailbox. The questionnaire was anonymous, and a relaunch was carried out by email and during the care team meetings 2 weeks after the first mailing. The care teams had 1 month to respond to the satisfaction survey. The questions covered different aspects: the respondent's profession, the satisfaction regarding their cooperation with the CPT and their presence in the surgery unit, the quality of the information collected by the pharmacists, the way the Medication Reconciliation Forms were distributed, the patient safety, the safety when carrying out their job and whether or not there was a gain of time. Finally, they were asked if they wanted to return to the previous system and if they considered that the introduction of the CPT would be beneficial for other surgery units in the hospital. Moreover, a suggestion box was added for respondents to write their opinion freely.
Results
Evaluation of the proportion of patients processed by the pharmaceutical team
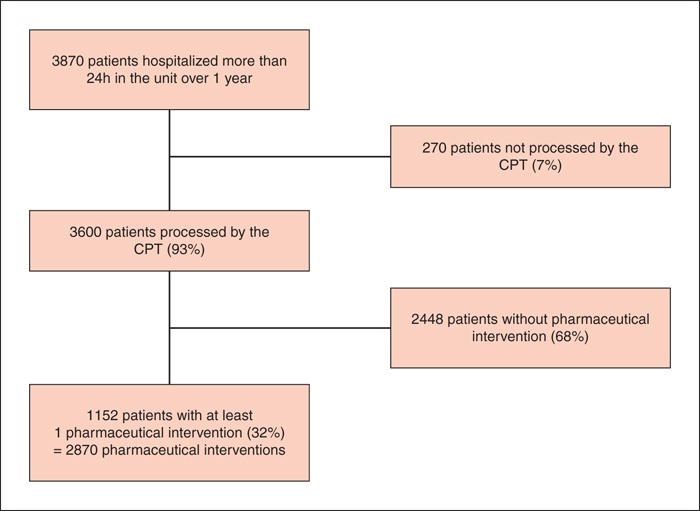
Over the course of a year, 3,600 patients have benefited from medication reconciliation (figure 1), which represents 93% of the patients who were hospitalised in the service more than 24 hours. The patients were 66,8 years old in average [standard deviation=17.8], with extremes of 15 and 116 years. Mean number of drugs per patient was 7, with a breakdown per age illustrated in table 1. It increased from 3.50 drugs when aged 15 to 25, until 9.40 when 75 to 85, and then decreased. The correlation coefficient for the number of drugs between 25 and 85 years old was 0.967 (R2=0.935).
Evaluation of the pharmaceutical interventions
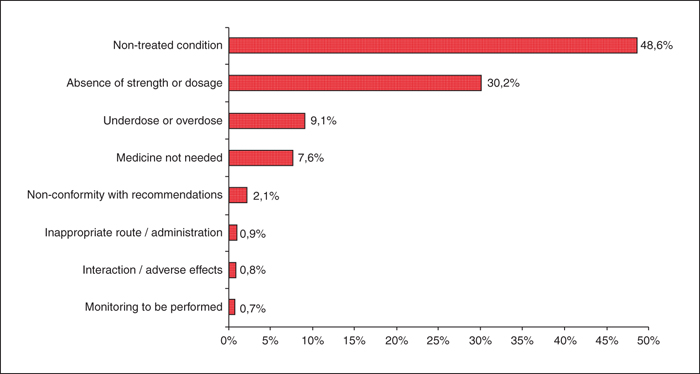
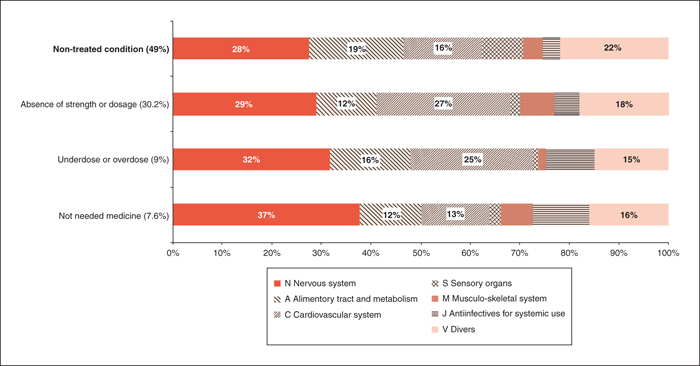
Out of 3,600 patients, 32% benefited from a pharmaceutical intervention (figure 1); 2,870 pharmaceutical interventions were carried out, the great majority (90.4%) done during medication reconciliation, the rest during hospitalization (medication review, pharmaceutical notifications and advices). The mean number of pharmaceutical interventions (PI) raised steadily from 0.2 per patient when patients were aged 15 to 25, to 1.4 per patient when aged 75 to 85 (table 1). It then decreased to reach 0.4 PI in patients aged more than 95 years of age. Ninety-six percents of the interventions had been accepted by the prescriber resulting in a modification of the prescription. The average (49%) of these interventions aimed to re-establish one or more forgotten drugs during the prescribing process in the surgery unit (figure 2); 39% of the pharmaceutical interventions consisted on correcting the absence of dosage or strength, or suggesting a modification of it.According to the ATC classification (Anatomic, Therapeutic and Chemical) [19], nervous system (30%) and cardio-vascular disease (20%) drugs were the most implicated drugs in the pharmaceutical interventions, followed by alimentary tract and metabolism drugs (15%) (Supplemental table). Nervous system drugs were more implicated when it came to stopping a not needed medicine (37%) and cardio-vascular drugs when a precision in dosage or strength was needed (27%) (figure 3). Twenty-five percents of the PIs were considered as severe errors.
Evaluation of the impact of medication errors declarations
Before the introduction of the CPT in the surgery unit, 27 medication errors had been reported in the previous 10 months. These errors exclusively involved the prescribing stage and were considered as highly critical in 78% of the cases. Extreme criticality was reached twice (3.7%) (table 2). Ten months following the introduction of the CPT, 7 medication errors had been noticed, thus this meant a 74.1% fall in the occurrence of these events. Moreover, only 1 out of 7 cases were of extreme or high criticality (-82,5%).
Satisfaction evaluation
Forty-seven healthcare professionals in the orthopaedic surgery unit (out of 78, 60.2%) responded to the survey (53.2% nurses, 23.4% surgeons, 14.9% anaesthetists, 8.5% others). They were mostly satisfied about the introduction of the CPT in the surgery unit and confirmed that this service would be beneficial for other surgery units (table 3). Moreover, a positive impact in patient care had also been noticed, and more than 9 people out of 10 (94%) would not go back to the previous organisation. The survey suggestions also reflected the overall satisfaction. It was mentioned that the CPT skills were an advantage, improved the quality of patient care, improved the safety of the prescriptions, saved time for the nurse and medical staff, and provided a better data transmission between the hospital and the general practitioners.
Discussion
Pharmaceutical interventions and therapeutic optimisation
We proved that the incorporation of a pharmaceutical team within an orthopaedic surgery unit allowed drug treatment to be safer due to the modifications in prescriptions from one out of three hospitalised patients. The rate of pharmaceutical interventions (32%) does not contradict the results found in the literature, which can be extremely variable between centres. However, it is difficult to show that reduction in medication errors had a clinical impact for the patient. The high number of patients seen by the CPT shows the benefit of having pharmacists that are fully involved in the clinical service for medication reconciliation and therapeutic optimisation (medication review, participation in clinical staffs, advices about pharmaceutical questions). In the future, pharmacy technicians could be involved in the medication reconciliation, their role being already demonstrated in preoperative screening [20].
The studied population, with an average age of 66.8 years and 7 medicine consumed is comparable to the other studies published about medication reconciliation [21, 22]. This activity has taken place in a context where patients are relatively old, often having multiple pathologies and drugs, therefore more likely to be subject of medical iatrogenesis [23-25].
We saw that the number of PI increased with the age until 85 years of age, and with the average number of medicine per person. It goes to the sense of the literature which shows that these criteria are often associated with a higher proportion of patients with discrepancies on admission [26-28]. Surgery departments are particurlay at risk with even discrepancies in preoperative medication histories between surgical and anesthesia records [26, 29]. The decrease in the number of PIs per patient over age 85 can be explained in two ways: these patients consume fewer drugs beyond this age (figure 3) [23] and most are institutionalized. Their medical records are therefore more reliable, and fewer errors occur during transitions.
The most common prescriptions modified by the CPT were related to cardiovascular and nervous system diseases. In addition to being the most prescribed, these medicinal classes are frequently incriminated as being suppliers of medicinal errors [30, 31], special attention is therefore paid to these therapeutic classes during medication reconciliation and medication review.
Most of the pharmaceutical interventions were related to forgotten prescriptions at the entry of patients to hospital or to dosage modifications. These results are similar to the ones from previous studies carried out in other centres [32, 33]. The acceptance rate of PIs is higher than that found in the literature (70-80%) [34-36]. This can be explained by the fact that the pharmaceutical team proposes to renew or modify the treatment directly on the prescription medium, requiring only the validation by the doctor. This is a good indicator of relevance and impact of pharmacists’ activities in the surgery unit. In addition, anaesthetists are dedicated to the orthopaedic surgery department. This allows a significant involvement in the management of prescriptions, and a long-term relationship with clinical pharmacists. We believe that the communication between pharmacists and prescribers should always be direct, instead of just relying on a computerised transmission [14, 37]. According to the literature, clinical pharmacists reduce the hospitalisation duration, the mortality and the rate of readmission [38-40], as well as improve the rate of appropriate antibiotic prophylaxis [41].
Medication errors
This study shows a decrease in the number of critical medication errors after the introduction of the CPT, even though the staff was sensitized to declaring during the same time. Medication reconciliation was associated with fewer medication errors caused by admission prescribing changes that were errors, as found in the literature [21, 42].
Adverse drug events would be the cause of 15.6% of the hospital direct expenses and of 18.6% of hospitalisation costs [43]. The presence of a CPT causes a decrease in drug costs [34, 44], especially antibiotics [45], as well as a reduction in avoided costs [34, 35, 46], even when the supplemental cost of pharmacist salaries is taken into consideration. It would be interesting in the future to carry out an economical study to evaluate the financial benefit resulting from the decrease in the incidence of adverse drug events in patients in surgery units.
Satisfaction
The satisfaction rate of the nursing and medical staff shows the positive opinion of the majority regarding to the CPT contribution to the surgery unit. According to the interviewees, CPT improves the medication circuit safety and the patient care, and saves time for the rest of the staff, allowing them to be more dedicated to carry out their job. The nursing and medical staff did not wish to go back to an organisation without CPT. This observation is frequently documented in the literature and proves that incorporated pharmacists are considered as an added value to the health care quality [32, 43, 44].
Study limitations
Although improvements in the health care were noted, these findings are a trend that needs to be verified and approved. Actually, this study suffers some methodological lacks as there is no control arm to assess the specific impact of the clinical pharmacist in the surgery unit. This weakness is one of many conclusions of many reviews [7, 8, 47] which state that rigorously designed studies comparing different inpatient medication reconciliation practices and their effects on clinical outcomes are scarce. However, indicators of effectiveness of routine care activities being variable and complex, the strength of this study lies in the large number of patients seen by the pharmaceutical team.
Moreover, the number of medication errors was based on voluntary reporting from the staff. It was technically difficult to evaluate the true occurrence of medication errors. However, the clinical staff remained the same during the study, and was not aware of the study.
Conclusion
To sum-up, the full-time presence of a pharmaceutical team in an orthopaedic surgery unit allows to take charge of all the patients that are meant to stay over 24h in the unit. The full-time presence of the CPT makes it easier to connect with physicians, and thus to gain acceptance of the pharmaceutical interventions. It leads to the decrease of medication errors. As it shows a gain in time and a global satisfaction among the staff, this type of organisation may be a solution to secure the medication circuit. Further intervention studies specifically designed to assess the impact of a clinical pharmacist in a surgery unit are needed to quantify the importance of these findings on clinically significant improvements.
Highlights
What is already known on this subject:
- –The involvement of a pharmacist in a clinical unit allows a better medication safety, due to different activities as medication review, medication reconciliation, and therapeutics optimization.
- –The majority of clinical pharmacy activities have been described in medical units with a large number of drug prescriptions such as geriatrics.
What this study adds:
- –Full time pharmacists in a surgery unit permit exhaustive medication reconciliation, and no studies to date have been conducted on as many patients and pharmaceutical interventions in the surgical sector.
- –The implementation of pharmacists in a surgery unit results in a decrease of medication errors, in numbers and criticity.
Annexe A Appendix
Acknowledgements
Ethics approval: This study received the approval of the local ethics committee (GNEDS, Nantes’ Group of Ethics in Health, 2015).
Conflict of interest: none of the authors has any conflict of interest to disclose concerning this article.
We thank all the members of the pharmaceutical, surgery and anaesthesiology teams for their participation in this study.
![]() Cette œuvre est mise à disposition selon les termes de la
Licence Creative Commons Attribution - Pas d'Utilisation Commerciale - Pas de Modification 4.0 International
Cette œuvre est mise à disposition selon les termes de la
Licence Creative Commons Attribution - Pas d'Utilisation Commerciale - Pas de Modification 4.0 International