Epileptic Disorders
MENUMedication-resistant acute focal motor seizures in a child with COVID-19 affecting the CNS Volume 24, numéro 5, October 2022
Several neurological conditions are known to be associated with COVID-19. Recent studies have indicated a strong link between COVID-19 and meningitis, encephalitis, acute disseminated encephalomyelitis, stroke, and even polyneuropathy in children [1-3]. Some paediatric patients with COVID-19 have been reported with acute symptomatic seizures without other manifestations of encephalitis or meningitis [4, 5], however, the main pathophysiological mechanisms of these seizures have yet to be established. This report describes a perfectly healthy girl who presented with acute repetitive focal aware motor seizures, while her brain MRI showed a lesion in the left posterior cortex. After a number of investigations, real-time RT-PCR for SARS-CoV based on cerebrospinal fluid (CSF) was positive. Despite receiving at least four anti-seizure medications at appropriate dosages, the patient’s seizures continued, and just after administering intravenous immunoglobulin (IVIG), her seizures stopped. This dramatic response to IVIG may indicate a hypothetical inflammatory process in the patient’s cortex caused by COVID-19.
Case study
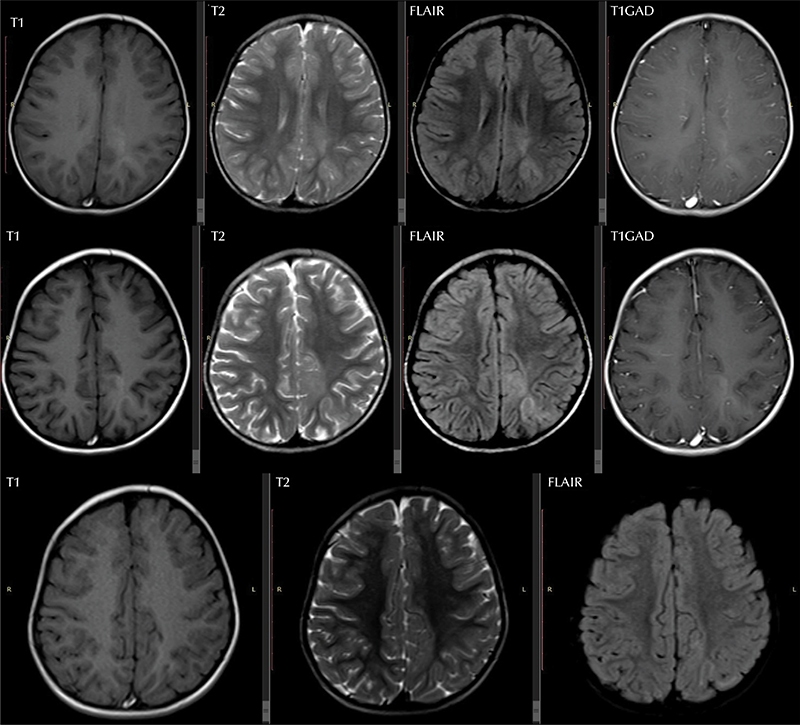
A girl aged three years and three months, who was perfectly healthy before her complaint, was referred to our centre due to medication-resistant focal motor seizures. Her problem had begun about 30 days before the referral. According to her mother, after going to a street food vendor and eating falafel among the crowd, she developed vomiting then diarrhoea on the same night. The next day, she convulsed with head version and facial twitches, but her mother did not take them seriously. Her mother described her events as head and neck version to the left, blinking, and facial twitching. The frequency of these seizures increased from 2-3 to more than 10 times in a day. At first, her parents refused to bring her to a medical facility because of fear of COVID-19 patients in hospitals, but as her condition worsened, her parents decided to bring her to the emergency department (ED), and after the first visit to the ED, she was admitted to Abuzar Children’s Hospital;the main general children’s hospital in Ahvaz (south-west of Iran). During hospitalization, she developed repeated focal aware motor seizures. She received anti-seizure medications to control her seizures, but seizures were unresponsive to IV phenobarbital, IV phenytoin, IV levetiracetam, and IV valproate. After 10 days of admission, her seizures were unresponsive to anti-seizure medications, and her parents decided to discharge her and go home. She stayed at home for 10 days, but due to the frequent seizures, she was referred to our hospital (Golestan hospital), which is a tertiary child neurology and epilepsy centre. She was the only child of a firstcousin marriage. Her perinatal and postnatal history were unremarkable. Her growth and development were acceptable, and her vaccination was up to date. Her systemic and neurological examinations were completely normal, and no fever was registered at admission and during the whole course of hospitalization. Her seizures were classified as focal aware motor seizures, which were accompanied by head and neck version to the right. These events lasted 30-40 seconds, and between seizures, she was completely normal. No Todd’s paralysis was seen after these events. Her laboratory data were normal, including; complete blood count, biochemistry, urine analysis and culture, cerebrospinal fluid (CSF) analysis and its bacterial culture, and chest X-ray. Her brain MRI showed a focal lesion in the left posterior cortex (figure 1; upper panel), and her video-EEG monitoring confirmed motor seizures. Anti-seizure medications, including IV phenytoin, IV levetiracetam, IV valproate, and oral clobazam at appropriate dosages, did not control her seizures. During her work-up, other results were obtained. Real-time RT-PCR for SARS CoV of the nasopharynx, as well as plasma, was negative, but was positive based on CSF. According to these results, we decided to administer 400 mg/kg/day intravenous immunoglobulin (IVIG) for five days. Her seizures were significantly reduced by infusing IVIG, and after three days, her seizures stopped. Two weeks after admission in our centre, serum IgG and IgM for COVID-19 were negative. Three weeks after admission, she was discharged on oral levetiracetam, clobazam, and valproate. During follow-up visits with monthly intervals, she was completely normal and seizure-free. One-year after the presentation of focal seizures, her clinical examination was normal, but follow-up brain MRI showed interesting changes (figure 1; middle and lower panel).
Brain MRI at the first admission showed abnormal signal changes in the left parieto-occipital cortex (figure 1; upper panel), but the following brain MRI (figure 1; middle and lower panel) showed different patterns of signal changes at the same anatomical region. The last MRI scan showed signal changes that were not seen on the first MRI scan (figure 1; lower panel). These signal changes on the first MRI scan appeared as new pathological signs in the patient’s brain, and the findings on the last MRI scan were considered to be structural changes due to the pathological process after a direct insult to the brain tissue by the virus.
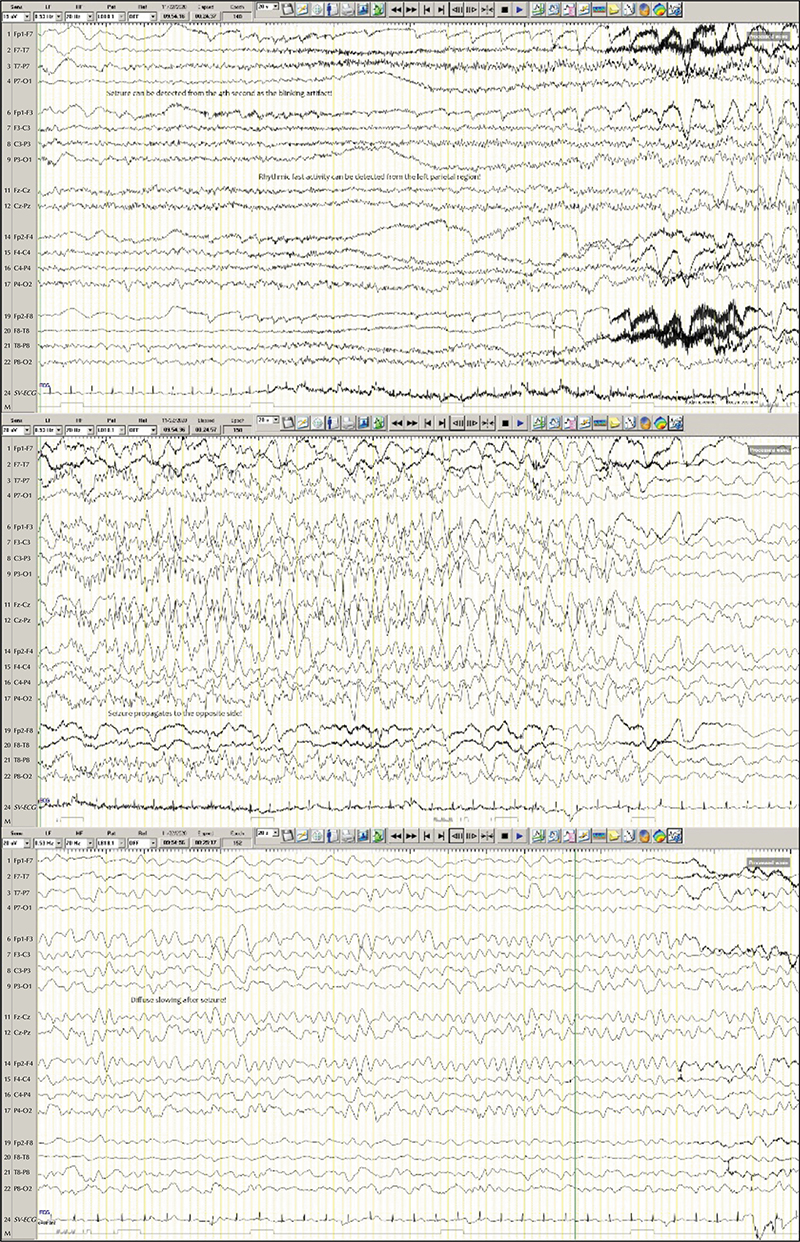
During hospitalization in our centre, we performed short video-EEG monitoring (VEM), and we succeeded in capturing at least one event in this child. Her VEM showed findings that were consistent with the brain MRI findings. The posterior dominant rhythm (PDR) was acceptable for her age (6-7 Hz at the parieto-central regions) and was reactive to eye opening and closure. In addition to abnormal nonpersistent polymorphic delta activity (PDA) at the left parieto-occipital region, we also identified scattered and infrequent epileptiform discharges in the same region. We could describe her event as bilateral blinking, followed by a dystonic posture of her right upper limb, and subsequently a short clonic movement was seen affecting the left upper limb. This event lasted for about 90 seconds, but our EEG technician did not succeed in assessing her awareness during this event. According to the anatomical region of the part of the brain involved, this seizure semiology would be caused by mesial and lateral involvement of the frontal networks of the same side. The EEG findings during this event were consistent with the brain MRI lesion, and we could determine a low-amplitude fast (about 12 Hz) rhythmic pattern from the left posterior cortex (P7, P3). This rhythmic activity propagated to the contralateral right region after 10 seconds, however, during this event, the bitemporal regions were not involved diffusely. We classified this seizure as a focal (possibly aware) motor tonic to clonic seizure (figure 2).
This case study indicated a number of clues that led us to consider a probable new insult in an otherwise healthy brain, leading to acute symptomatic seizures, and these clues are outlined below. According to her mother, she was completely normal before these seizures, therefore, she must have suffered a new insult to her brain. After reviewing her brain MRI, we considered focal cortical dysplasia (FCD), as she began to show focal motor seizures. However, her VEM and the following MRI scans were not consistent with this hypothesis. As stated previously, during VEM, we determined PDA but no repetitive consistent epileptiform discharges (the interictal EEG signature of FCDs) [6, 7], and this finding on EEG does not indicate the possibility of FCDs. In addition, the following MRI scans showed changes in the brain lesion, and we know that in this age range brain MRI findings of FCDs are fairly consistent and static. After a comprehensive literature search, we could not find any report describing the same MRI findings as in our patient. We therefore recommend adding posterior cortex involvement to the previously documented neuroradiological findings in children with cerebral involvement of COVID-19 [1]. In summary, both brain MRI and VEM findings indicated a new brain insult in this patient.
The patient was referred to our hospital during the fourth wave of COVID-19 (after the breakthrough of COVID-19 caused by the delta variant) in our country, therefore, investigating the source of COVID-19 in this child was logical. From an epidemiological viewpoint, she had been in a crowd with many patients who may have had COVID-19 on the day of her visit. Logically, she must have been infected before this visit because she developed her symptoms on the night of her visit. It is possible that she was in contact with asymptomatic people with COVID-19, but her mother was unable to confirm this. Unfortunately, after identifying COVID-19 in this child, and according to her presentation, we did not extend our investigations to rule out other probable viral causes. Therefore, we have no information on other viral causes of acute CNS insults in this child, and this was a failure in this child. In addition, a number of reports have claimed cross-reaction between different kinds of coronaviruses in humans [8]. Surprisingly, we could not find any report of PCR-positive CSF in a child without severe manifestations of COVID-19 [1-3, 9]. Therefore, positive RT-PCR for SARS-CoV-2 in the CSF of this child might be merely a coincidental finding or even a false-positive result.
In a recently published study, the different causes of false-positive SARS-CoV-2 RT-PCR results have been discussed [10]. The list of causes of false-positive results is exhaustive, but the main causes are; contamination during sampling, extraction and PCR amplification; contamination of the equipment by high-viral-titre specimens; cross-reaction with other viruses; sample mix-ups; software problems; data entry or transmission errors; miscommunicating results; variations in parameters around the limit of detection and definition of an indeterminate result; assuming that an indeterminate result is positive; and non-specific reactions. Fortunately, an algorithm exists which aids the decision of what to do when faced with a patient with a probable false positive SARS-CoV-2 RT-PCR result [10]. According to this algorithm, when the patient had a high risk of exposure or has symptoms compatible with COVID-19, we can assume that the result is a true positive. In summary and according to this study, our patient had a high risk of exposure to COVID-19 patients, therefore, considering her to have true cerebral involvement of COVID-19 was logical.
The final evidence that we must consider is that despite receiving at least four anti-seizure medications at appropriate dosages, her seizures continued, and just after administering IVIG, her seizures stopped. This dramatic response to IVIG may indicate a hypothetical inflammatory process in her brain. We should emphasize that during hospitalization, she did not show any signs or symptoms of respiratory involvement, and according to COVID-19 treatment protocols in our centre, we did not administer Remdesivir. During follow-up, we decided to investigate a COVID-19 antibody response in this child, but the results were negative. We know that IVIG infusion can induce immunosuppression by suppressing the proliferation of B lymphocytes and, thus, modulation of antibody production [11]. IVIG can also suppress autoreactive B lymphocytes and neutralize their cytokines [12].
In conclusion, this interesting presentation of COVID-19 in a previously completely healthy girl expands our knowledge about the neurological manifestations of COVID-19 in children. This study indicates that COVID-19 can present as merely acute focal motor seizures in children [4, 5]. Different mechanisms of seizures have been suggested in patients with COVID-19 [13], but in this girl, primary involvement of the cortex and an inflammatory response might have been the main mechanisms.
Test yourself
- A strong link between COVID-19 and which of the following conditions has been indicated?
- Encephalitis
- Acute disseminated encephalomyelitis
- Stroke
- Polyneuropathy
- All of the above
- According to the literature, PCR for SARS-CoV-2 in CSF is always positive.
- True
- False
- True in children
- True in adults
- Which statement is correct?
- Seizures in children with cerebral involvement of COVID-19 are always accompanied by fever.
- Lungs are always involved in children with a COVID-19-affected CNS.
- Seizures in children with a COVID-19-affected CNS are responsive to anti-seizure medications.
- Seizures in children with a COVID-19-affected CNS always have a generalized onset.
- None of the above
Note: Reading the manuscript provides an answer to all questions. Correct answers may be accessed on the website, www.epilepticdisorders.com.
Supplementary material
Summary slides accompanying the manuscript are available at www.epilepticdisorders.com.
Disclosures
None.