Epileptic Disorders
MENULong-lasting seizure-related anxiety in patients with temporal lobe epilepsy and comorbid psychiatric disorders Volume 17, numéro 3, September 2015
Diagnosis and management of comorbid anxiety disorders is an important issue in patients with epilepsy (Beyenburg et al., 2005). As for comorbid depression, comorbid anxiety disorders are associated with poor quality of life, increased risk of post-operative psychiatric disturbances, and poor post-operative seizure outcome in patients who undergo epilepsy surgery (Kanner, 2013).
Their characterization relies on specific criteria enumerated in the Diagnostic and Statistical manual of Mental disorders (DSM-V) of the American Psychiatric Association (2013). In patients with epilepsy, specific attention should be paid to differentiate between symptoms related to anxiety disorders and seizure-related symptoms. Although seizures associated with ictal anxiety (IA) and acute anxious episodes, such as panic attacks (PA), might share many symptoms, including chest or abdominal discomfort, “losing-control” feelings, paresthesia, and vegetative symptoms, they may be distinguished with the help of several clinical characteristics (Handal et al., 1995). Anxiety in PA is typically intense and resolves gradually in several minutes, whereas IA is usually moderate, brief (<120 s), and accompanied by other symptoms, such as impairment of consciousness and automatisms. In some patients, these criteria might, however, be misleading, especially when symptoms are observed over hours or days. Here, we report two patients with drug-resistant temporal lobe epilepsy (TLE) who developed long-lasting seizure-related psychiatric symptoms, suggestive of exacerbation of comorbid anxiety disorder.
Case studies
Patient 1
Patient 1, a 43-year-old, right-handed woman, suffered from drug-resistant right-sided TLE. Seizures were characterized by an ill-defined internal sensation associated with fear, followed by loss of awareness, oro-alimentary automatisms, pallor, and tachycardia. MRI showed right hippocampal atrophy. The patient underwent right mesial temporal gamma knife radiosurgery (GKS) that failed to control seizures. In parallel, she developed depression and anxiety disorders, the severity of which varied depending on seizure frequency. Four years after radiosurgery, she underwent stereotactic intra-cerebral EEG (SEEG) recordings with the hope of delineating the regions responsible for the ongoing seizures. Details of the SEEG protocol and data observed in this patient, a pattern of subcontinuous spiking activity intermingled with asymptomatic rhythmic discharges within the irradiated structures, have been previously reported (Rheims et al., 2011). During SEEG monitoring, the patient developed an unusually intense and prolonged anxious episode that began with a feeling of losing control. Anxiety progressively increased over one hour. The symptoms fluctuated and the patient demonstrated alternating laughter and tears (video sequence 1). Progressively, she reported chills, diffuse paresthesia, dizziness, nausea, and vertigo. She was polypnoeic throughout the episode. However, she remained free of any of the objective clinical signs usually observed during her seizures. She was fully conscious and able to interact with the staff. As shown in table 1, the symptoms fulfilled the DSM-V criteria for PA and were not recognized as seizure-related, neither by the patient, who had experienced similar anxious episodes lasting from a few seconds to a few minutes, nor by the trained staff. One hour after the onset of symptoms, the patient became dysarthric and developed left facial contraction preceding secondary generalization. SEEG recordings showed that the anxiety symptoms were associated with an epileptic discharge that remained restricted to the temporo-basal cortex. She underwent right anterior temporal lobectomy and has been seizure-free for seven years. No acute psychiatric episode occurred after surgery.
Patient 2
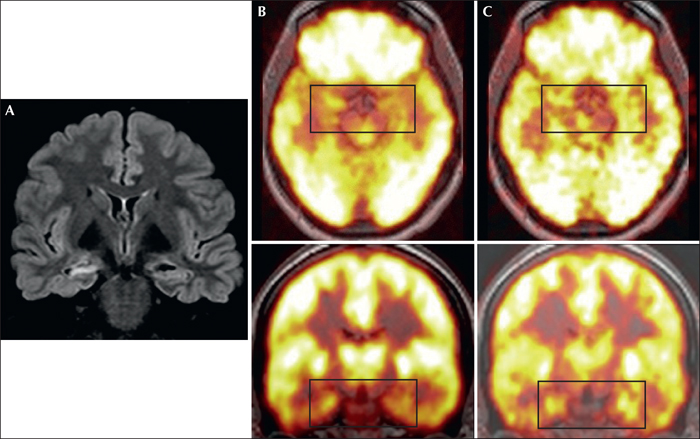
Patient 2, a 23-year-old, right-handed woman, suffered from drug-resistant right TLE. She had a history of complex febrile seizures during childhood. Seizures were characterized by an intense fear sensation and thoracic oppression, followed by partial loss of awareness with verbal and gestural automatisms. Secondary generalizations were frequent. MRI showed right hippocampal atrophy (figure 1A), and interictal and ictal EEG pointed to the right temporal lobe. Despite these electroclinical data, and because of psychiatric symptoms, epilepsy surgery was initially not considered suitable. She indeed suffered from severe psychiatric comorbidities, including depression associated with generalized anxiety and cluster B personality disorder traits, mainly impulsivity and low frustration tolerance (American Psychiatric Association, 2013). The socio-familial environment was unstable with recurrent familial conflicts and exclusions from reception centres. Exacerbation of psychiatric symptoms frequently required admission to psychiatric settings, some involuntary due to severe aggressiveness and violence. During one of these episodes, and while the psychiatric symptoms worsened over a week, she was admitted to our unit where she demonstrated extreme difficulty in managing her emotions with frequent temper tantrums and continuous intense anxiety. However, she also reported mild rising thoracic oppressions, several times per hour. Concomitant scalp-EEG failed to show any ictal activity but [18F] FDG-PET revealed an asymmetry within the limbic structures with relative hypermetabolism of the right mesial temporal lobe, in comparison with the contralateral structures (figure 1B). Following high-dose clobazam for a week, anxiety progressively resolved. [18F] FDG-PET was controlled three months later and showed a clear-cut right mesial temporal lobe hypometabolism (figure 1C), suggesting that the initial [18F] FDG-PET pattern reflected a peri-ictal state during which frequent epileptic discharges might have driven the anxiety symptoms. The patient eventually underwent right anterior temporal lobectomy and has now been seizure-free for 14 months. Psychiatric symptoms also improved post-operatively without recurrence of marked anxiety disorder.
Discussion
The two patients reported herein highlight the difficulties in distinguishing ictal from interictal anxiety disorders in some patients with mesial TLE, especially in those who suffer from psychiatric comorbidities.
IA is frequently reported during focal seizures, especially when originating within the non-dominant temporal lobe (Sazgar et al., 2003). In our patients, the ictal origin of anxious symptoms could not be fully ascertained. In Patient 1, psychiatric symptoms were associated with temporo-basal discharges, but GKS-induced modifications of the epileptogenic network hampered straightforward electroclinical correlations (Rheims et al., 2011). Patient 1 used to experience similar anxious episodes, but of shorter duration. The noteworthy long duration of the reported seizure might have been favoured by the reduction of the dosage of antiepileptic drugs to promote a timely occurrence of seizures during SEEG. In Patient 2, repetitive rising thoracic sensations in association with transient relative hypermetabolism within the epileptogenic temporal lobe were suggestive of focal status epilepticus (Meltzer et al., 2000), but direct EEG evidence was lacking.
Anxiety involves a distributed network of interconnected structures that primarily include the amygdala, the hippocampus, the anterior cingulate gyrus, and the prefrontal and orbitofrontal cortices (Stahl, 2003). IA can be observed in seizures involving all or part of this network (Biraben et al., 2001). Although direct activation of the amygdala can elicit fear (Gloor et al., 1982), it has also been suggested that acute alteration of emotional behaviour in seizures might result from the transient desynchrony of emotion-regulation networks (Bartolomei et al., 2005). Whether the anxiety observed in our patients reflected the spreading of epileptic discharges within the brain structures involved in the control of emotions, or a transient disruption of this network in the context of repetitive temporal lobe seizures, remains an open question. In any case, seizures likely triggered the anxiety symptoms and had to be treated in order to improve the latter.
Several authors have reported detailed analyses of seizures where anxiety remained isolated (Wieser et al., 1985; Spitz, 1991). IA is typically characterized by a sudden onset, a short duration (i.e. <5 minutes), stereotyped symptoms, and partial alteration of consciousness, with or without other psychological or autonomic features of temporal lobe seizures (Beyenburg et al., 2005). In contrast, anxiety episodes of long duration, or those with intensity which is influenced by external factors, are usually considered unlikely to be seizure related. These clinical characteristics did not apply to our two patients. The first part of Patient 1's episode was misleading, due to its duration and semiology (see table 1), and to the positive influence of the nurses’ reassuring attitudes towards the intensity of the symptoms. Similarly, Patient 2 demonstrated anxiety over several days, in association with other psychiatric symptoms highly influenced by external factors.
Importantly, the erroneous determination that these symptoms were of psychiatric origin was influenced by the baseline psychiatric condition of both patients. Both suffered from psychiatric comorbidities and Patient 2 had been hospitalized periodically because of similar transient aggravation of anxiety symptoms.
The presence of psychiatric comorbidities increases the risk of unfavourable surgical outcome, both in terms of seizure control and psychiatric status (Kanner, 2013). Accordingly, epilepsy surgery was not initially considered for Patient 2 due to her psychiatric instability and behavioural problems. However, it might be speculated that most of her previous psychiatric decompensations were also related to long-lasting intralimbic seizure activity. As a matter of fact, no such episodes recurred after epilepsy surgery and the psychiatric comorbidities improved. Earlier recognition of the link between seizure activity and psychiatric symptoms might thus have led to earlier surgery.
The relationship between epilepsy and anxiety disorders is complex; epileptic activity can mimic anxious episodes even when the psychiatric semiology is prolonged and isolated. Management of psychiatric episodes among patients with epilepsy requires cautious neurological investigation.
Supplementary data
Summary didactic slides are available on the www.epilepticdisorders.com website.
Disclosures
None of the authors have any conflict of interest to disclose.