Epileptic Disorders
MENUKnowledge gaps for functional outcomes after multilobar resective and disconnective pediatric epilepsy surgery: Conference Proceedings of the Patient-Centered Stakeholder Meeting 2019 Volume 24, numéro 1, February 2022
- Mots-clés : pediatric epilepsy, hemispherectomy, hemispherotomy, multi-lobar epilepsy surgery, functional outcome
- DOI : 10.1684/epd.2021.1373
- Page(s) : 50-66
- Année de parution : 2022
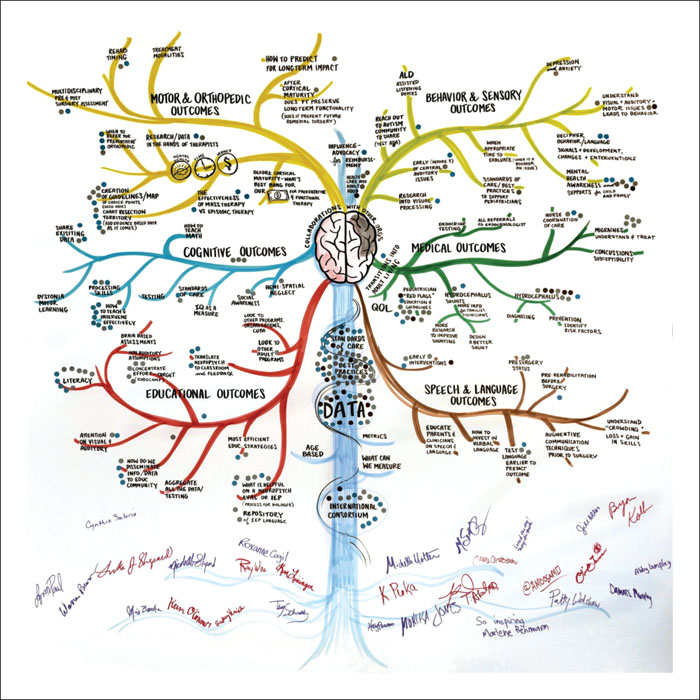
For children with medication-resistant epilepsy who undergo multilobar or hemispheric surgery, the goal of achieving seizure freedom is met with a variety of potential functional consequences, both favorable and unfavorable. However, there is a paucity of literature that comprehensively addresses the cognitive, medical, behavioral, orthopedic, and sensory outcomes across the lifespan following large epilepsy surgeries in childhood, leaving all stakeholders underinformed with regard to counseling and expectations. Through collaboration between clinicians, researchers, and patient/caregiver stakeholders, the “Functional Impacts of Large Resective or Disconnective Pediatric Epilepsy Surgery: Identifying Gaps and Setting PCOR Priorities” meeting was convened on July 18, 2019, to identify gaps in knowledge and inform various patient-centered research initiatives. Clinicians and researchers with content expertise presented the best available data in each functional domain which is summarized here. As a result of the meeting, the top three consensus priorities included research focused on postoperative: (1) hydrocephalus; (2) mental health issues; and (3) literacy and other educational outcomes. The proceedings of this meeting mark the first time research on functional outcomes after resective and disconnective pediatric epilepsy surgery has been codified and shared among multidisciplinary stakeholders. This joint initiative promotes continued collaboration in the field and ensures that advancements align with actual patient and family needs and experiences. Collaboration around common objectives will lead to better informed counseling around postoperative expectations and management for children undergoing epilepsy surgery.