Epileptic Disorders
MENUImproved access to rapid electroencephalography at a community hospital reduces inter-hospital transfers for suspected non-convulsive seizures Volume 24, numéro 3, June 2022
- Mots-clés : hub-and-spoke model, tele-neurology, electroencephalography, rapid response electroencephalography, non-convulsive seizures, status epilepticus
- DOI : 10.1684/epd.2021.1410
- Page(s) : 507-16
- Année de parution : 2022
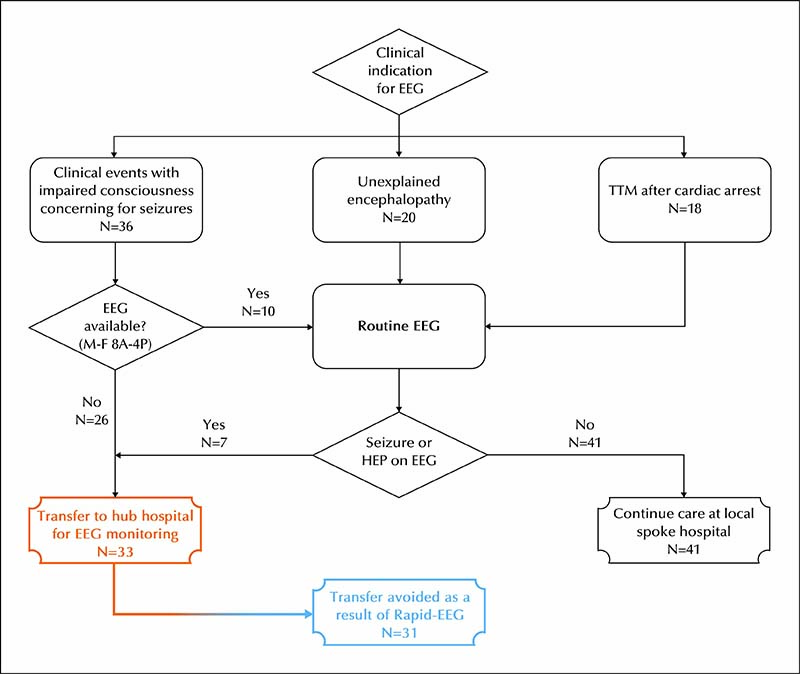
Objective. Patients with suspected non-convulsive seizures are optimally evaluated with EEG. However, limited EEG infrastructure at community hospitals often necessitates transfer for long-term EEG monitoring (LTM). Novel point-of-care EEG systems could expedite management of nonconvulsive seizures and reduce unnecessary transfers. We aimed to describe the impact of rapid access to EEG using a novel EEG device with remote expert interpretation (tele-EEG) on rates of transfer for LTM.
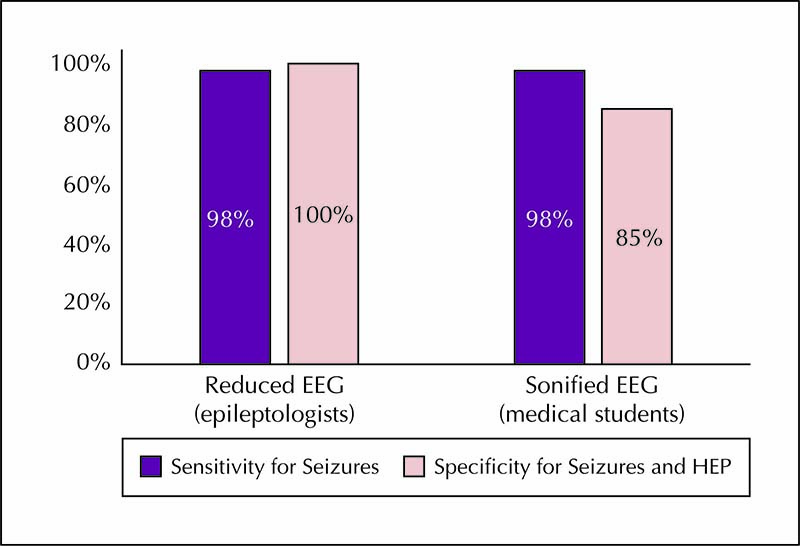
Methods. We retrospectively identified a cohort of patients who underwent Rapid-EEG (Ceribell Inc., Mountain View, CA) monitoring as part of a new standard-of-care at a community hospital. Rapid-EEGs were initially reviewed on-site by a community hospital neurologist before transitioning to tele-EEG review by epileptologists at an affiliated academic hospital. We compared the rate of transfer for LTM after Rapid-EEG/tele-EEG implementation to the expected rate if rapid access to EEG was unavailable.
Results. Seventy-four patients underwent a total of 118 Rapid-EEG studies (10 with seizure, 18 with highly epileptiform patterns, 90 with slow/normal activity). Eighty-one studies (69%), including 9 of 10 studies that detected seizures, occurred after-hours when EEG was previously unavailable. Based on historical practice patterns, we estimated that Rapid-EEG potentially obviated transfer for LTM in 31 of 33 patients (94%); both completed transfers occurred before the transition to tele-EEG review.
Significance. Rapid access to EEG led to the detection of seizures that would otherwise have been missed and reduced inter-hospital transfers for LTM. We estimate that the reduction in inter-hospital transportation costs alone would be in excess of $39,000 ($1,274 per patient). Point-of-care EEG systems may support a hub-and-spoke model for managing non-convulsive seizures (similar to that utilized in this study and analogous to existing acute stroke infrastructures), with increased EEG capacity at community hospitals and tele-EEG interpretation by specialists at academic hospitals that can accept transfers for LTM.