Epileptic Disorders
MENUChallenges in the first seizure clinic for adult patients with epilepsy Volume 18, numéro 3, September 2016
- Mots-clés : first seizure, seizure mimicker, psychogenic non-epileptic seizure, syncope, emergency referral epilepsy
- DOI : 10.1684/epd.2016.0853
- Page(s) : 305-14
- Année de parution : 2016
Aims. (1) To delineate the challenges in seizure diagnosis in the first seizure clinic setting for adult patients of a teaching hospital, and (2) quantify the diagnostic accuracy of the referral source and the yield of routine investigations, including blood tests, EEGs, and neuroimaging.
Methods. We retrospectively reviewed medical records of patients referred by the emergency department to the adult first seizure clinic and seen by the same epilepsy specialist between June 2007 and June 2011. The diagnostic accuracy in the emergency department was calculated by comparing with the final diagnosis made by an epilepsy specialist.
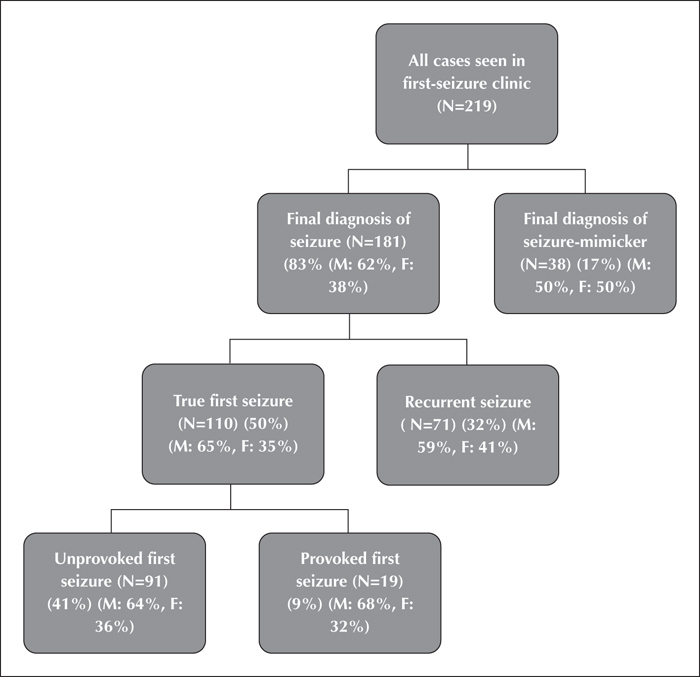
Results. In total, 219 patients were referred to the first seizure clinic. Median age was 45 and 60% of patients were male. From the cohort, 38 (17%) patients presented with seizure mimickers; the most common were reflex syncope (74%) and psychogenic non-epileptic seizures (16%). From the remaining 181 patients presenting with seizures, only 110 (61%) of these patients were diagnosed with true first seizures, and 71 (39%) patients had evidence of previous seizures. Nineteen (17%) of true first-ever seizures were provoked. The most frequent cause of provoked seizures was alcohol and illicit drugs (65%). In the emergency department, sensitivity and specificity in seizure diagnosis were 0.74 and 0.32, respectively.In our true first seizure patients, the EEG demonstrated epileptiform discharges in 22 (21%) patients. In the same cohort, computed tomography and magnetic resonance neuroimaging conferred 16% and 20% probability of finding a potentially epileptogenic structural abnormality, respectively. The most common epileptogenic abnormality found on magnetic resonance neuroimaging was cortical infarct.
Conclusions. The diagnosis and management of first seizure remains challenging due to the variety of seizure mimickers and low yield of investigations. Our data highlight the potential pitfalls and practical challenges in this process, as well as the need for these patients to be assessed in dedicated first seizure clinics.