Epileptic Disorders
MENUAcquired epileptic opercular syndrome related to a heterozygous deleterious substitution in GRIN2A Volume 19, numéro 3, September 2017
Epileptic encephalopathy with continuous spike-and-waves during sleep (CSWS), including Landau-Kleffner syndrome (LKS), is an epilepsy syndrome of childhood defined by the association of two features. The first is a cognitive or behavioural impairment acquired during childhood, unrelated to any factor in particular (e.g. prolonged and repetitive seizures, antiepileptic [AED] side effect, underlying metabolic or heredo-degenerative disease, or psycho-affective problem), other than the presence of abundant interictal epileptiform discharges (IEDs) during sleep. The second is focal or generalized IED during the awake state with strong activation and diffusion over the whole scalp during NREM sleep (for a review seeVan Bogaert, 2013). In LKS, receptive language is severely affected and typically consists of auditory verbal agnosia, with deterioration of understanding and use of words (Paquier et al., 1992). Within the spectrum of epileptic encephalopathy with CSWS, patients may show deterioration in oral motor function with preserved receptive language (Roulet et al., 1989; Deonna et al., 1993; Shafrir and Prensky, 1995). This entity is called “acquired epileptic opercular syndrome” (AEOS) (Shafrir and Prensky, 1995).
In 2013, three important parallel studies identified de novo or inherited deleterious variants of the GRIN2A gene in 9-20% of individuals affected by either epileptic encephalopathy with CSWS including LKS, or les severe phenotypes such as benign childhood epilepsy with centro-temporal spikes (BECTS) (Carvill et al., 2013; Lemke et al., 2013; Lesca et al., 2013). More recently, Turner et al. reported two families in which affected members had a combination of speech dyspraxia1 and dysarthria (Turner et al., 2015). The authors stated that this impairment of speech production was best explained by a dysfunction of NMDA receptors, as a consequence of the genetic variant rather than due to the associated epilepsy.
Here, we report a patient with a GRIN2A pathogenic variant with speech deterioration, leading to AEOS and the EEG pattern of CSWS, who dramatically recovered after treatment with hydrocortisone.
Case study
This 6-year-old male patient was the first child of non-consanguineous Belgian parents. His father presented with febrile convulsions in infancy, then seizures until age 13, and cognitive delay. On his paternal side, the patient's aunt and grandfather had imprecise histories of epilepsy.
The patient was born after a 38-week pregnancy with uncomplicated delivery. The first language skills were acquired at normal age except mildly delayed phonology. Seizures started at age 4 with a sleep-related febrile generalized convulsive seizure of 15 minutes. After a few months, non-febrile tonico-clonic seizures, lasting 2-3 minutes, occurred with a maximal rate of five seizures per month. Immediately after the first seizure, he started to present increasing difficulties in speech and learning.
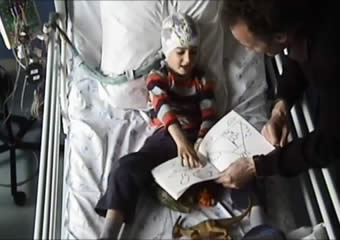
Clinical examination, which was normal after the first seizure, showed severe facial hypotonia with drooling and automatic-voluntary dissociation. The movements of the tongue and lips were very limited, hardly distinguishable from paresia and/or apraxia. He was almost speechless, except for some over-learned words such as “mummy” (video sequence 1). However, he was able to understand simple spoken language. Imitation of manual gesture was also impaired with dysdiadochokinesis. Attention was impaired.
Non-verbal intellectual ability was assessed using the WPPSI-III scale, showing a performance index of 56 and processing speed index of 45.
Figure 1 illustrates the results of the electrophysiological and functional neuroimaging investigations performed during the acute phase of CSWS. Interictal EEGs showed spike-wave discharges over the centro-parietal regions with variable bilateral spread when awake, and even more widespread and continuous during slow-wave sleep, corresponding to CSWS. Structural cerebral MRI was normal. Positron emission tomography with 18F-fluorodeoxyglucose (FDG-PET) was performed at rest when awake in the interictal state and under EEG control (see De Tiège et al. [2008] for more details). FDG-PET data were analysed using statistical parametric mapping (SPM8, http://www.fil.ion.ucl.ac.uk/spm/, Wellcome Trust Centre for Neuroimaging, London, UK). The patient's data were compared to a control group of young healthy adults using a previously reported method (De Tiège et al., 2008, 2013). Significant increase in relative glucose metabolism was found in bilateral superior parietal regions (pFWE<0.05). Magnetoencephalography (MEG), under sedation the same day as FDG-PET, revealed CSWS activity with independent onsets of epileptic discharges located in superior parietal or opercula regions bilaterally; superior parietal onsets were much more frequent than the opercular onsets (for more details on the methods used, see De Tiège et al. [2013]). Co-registration of MRI, MEG, and FDG-PET data revealed good anatomical concordance between superior parietal hypermetabolism and CSWS onsets.
Genetic analysis by targeted Sanger sequencing revealed a GRIN2A heterozygous substitution located in the donor splice site, in intron 3; c.1007+1G>A (RefSeq NM_ 000833). This variant was inherited from the patient's father. It is predicted to cause skipping of exon 4, resulting in a truncated protein. This variant has previously been reported in three unrelated families and is, so far, the most frequent deleterious variant reported for GRIN2A (Lemke et al., 2013).
Valproate was first initiated but quickly interrupted because of an exacerbation of attention deficits. Levetiracetam was tried, later combined with clobazam, but did not control the seizures. Hydrocortisone was then started at 5 mg/kg/day, and the scheme proposed by Buzatu et al. (2009) was followed for one year. This resulted in a dramatic improvement of speech after three months (video sequence 2). Both speech production and non-speech oral motor skills improved.
After three months of corticotherapy, he became seizure-free and this beneficial impact persisted after a two-year follow-up period. After three months, the EEG showed rare parietal IEDs when awake and a decrease in the spike-wave index from 100% to 50% during slow sleep, with an absence of spreading over the whole scalp.
Table 1 summarizes the evolution of language at 6 years of age before the hydrocortisone was started, and 20 months later. Twenty months after starting hydrocortisone, speech was intelligible even though a combination of dysarthria and speech apraxia persisted. Tongue movements were still limited during non-speech motor tasks. Mild speech apraxia still resulted in difficulty repeating trisyllabic sequences, which is characteristic of impaired motor speech planning and programming (Turner et al., 2015).
Discussion
To the best of our knowledge, this is the first well-documented case of Acquired Epileptic Opercular Syndrome (AEOS) associated with a deleterious GRIN2A variant, in which a mild pre-existing speech disorder showed dramatic deterioration triggered by epileptic activity. Corticotherapy resulted in impressive clinical recovery with seizure relief and disappearance of CSWS activity.
GRIN2A mutation is recognized as a major cause of LKS, in which language regression concerns both receptive and expressive modalities (Carvill et al., 2013; Lemke et al., 2013; Lesca et al., 2013). Another speech phenotype of GRIN2A mutation combines developmental dysarthria and speech dyspraxia with relative sparing of language comprehension (Turner et al., 2015). The absence of regression of motor speech is a cardinal feature that distinguishes this condition from AOES. However, a 5-year-old proband from a family with “autosomal dominant rolandic epilepsy with speech dyspraxia”, reported by Scheffer et al. (1995), and more recently reported to harbour a GRIN2A deleterious variant (Carvill et al., 2013), had a phenotype that was fairly similar to our patient, with acute non-speech oromotor apraxia within a context of global development delay. In this patient, the EEG demonstrated non-convulsive status epilepticus, probably corresponding to the CSWS definition. Furthermore, valproate temporarily improved speech impairment, but did not control the seizures.
Taken together, those two cases suggest an important pathophysiological role for epileptic discharges in the observed regression of speech. This hypothesis is further supported by the abnormal regional cerebral glucose distribution observed in the acute phase of the disease, with significant increase in relative glucose metabolism in bilateral superior parietal areas that co-localize with CSWS onsets. Indeed, we previously demonstrated the normalization of FDG-PET abnormalities in such conditions after successful treatment of CSWS with hydrocortisone (De Tiège et al., 2008).
AEOS is expected to result from dysfunction of the anterior opercular regions (Dronkers, 1996),but more recent data concluded that the neural basis for apraxia of speech is actually poorly understood (Liégeois and Morgan, 2012). In the present case, metabolic changes concerned superior parietal cortical areas and CSWS onsets involved superior parietal and opercular regions, bilaterally. The combination of superior parietal and opercular dysfunction probably led to speech apraxia.
In conclusion, this case strongly suggests that the speech impairment in patients with GRIN2A deleterious variants has a double origin. This is partially developmental due to a dysfunction of NMDA receptors, but at a later age, the emergence of an intense epileptic activity is prone to induce an acute and dramatic worsening of the speech disorder, especially when the epilepsy is complicated by CSWS (as in children with LKS who display a mild language delay before dramatic language regression). From this perspective, the GRIN2A-related epileptic spectrum is consistent with the definition of epileptic encephalopathy, i.e. a condition in which epileptiform abnormalities may contribute to progressive cognitive dysfunction. Early intervention may effectively improve developmental outcome.
Supplementary data
Summary didactic slides are available on the www.epilepticdisorders.com website.
Disclosures
The authors have no conflict of interest to disclose.
1 In our study, the term “speech apraxia” denotes an acquired disorder of motor speech planning and programming, whereas the term “speech dyspraxia” refers to the developmental variant of the speech disorder.