Epileptic Disorders
MENUEtiology and prognostic significance of ictal EEG patterns in patients with non-convulsive seizures Volume 24, numéro 1, February 2022
395 W. 12th Ave 7th floor, Columbus, Ohio 43210, USA
- Mots-clés : non-convulsive seizures, ictal EEG pattern, continuous EEG monitoring
- DOI : 10.1684/epd.2021.1363
- Page(s) : 75-81
- Année de parution : 2022
Objective
We aimed to study the ictal EEG patterns in patients with non-convulsive seizures (NCS) and their relationship with underlying etiology and patient outcome.
Methods
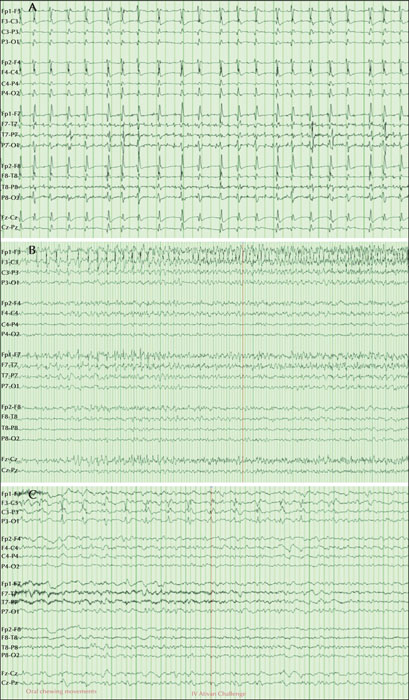
We conducted a retrospective review of EEG studies from patients undergoing continuous EEG (cEEG) monitoring for indication of altered mental status with a suspicion of NCS. Ictal EEG findings of NCS were categorized as three patterns: focal or generalized epileptiform discharges (EDs) at frequencies >2.5 Hz (Pattern 1); EDs at frequencies of ≤2.5 Hz or rhythmic activity >0.5 Hz with spatiotemporal evolution (Pattern 2); and EDs with ≤2.5 Hz with subtle clinical correlate during the ictal EEG or clinical and EEG improvement after a trial of IV anti-seizure drugs (Pattern 3). Patients with anoxic brain injury were excluded from the study. Associations between ictal EEG patterns and underlying etiology and their impact on in-hospital mortality was measured.
Results
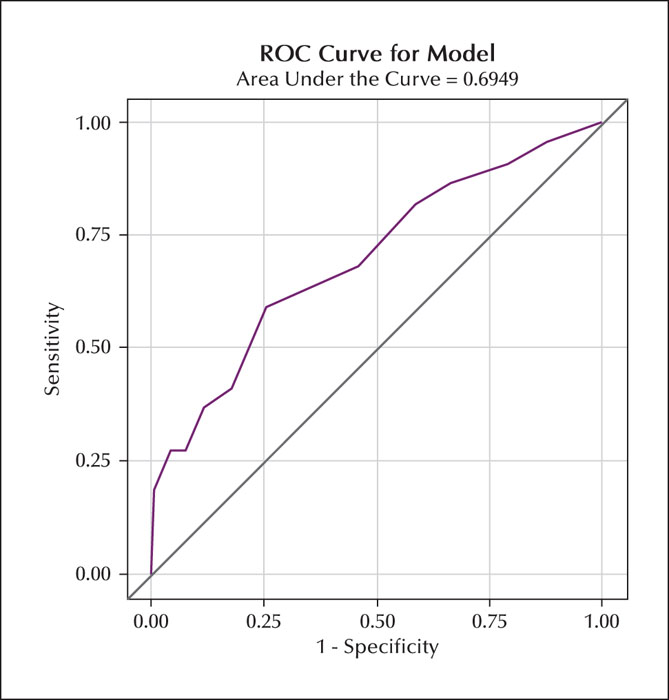
Of 487 patients included in the study, NCS was recorded on cEEG monitoring in 57 (12%). The ictal EEG Pattern 2 was the most commonly seen ictal EEG finding in our cohort of patients with NCS (70%, n=40/57), followed by Pattern 3 (15%, n=9/57) and Pattern 1(14%, n=8/57). In patients with acute brain injury, Pattern 2 (67%, n=27/40) was a commonly seen ictal EEG finding, whereas Pattern 1 (62% n=5/8) was seen in patients with underlying acute medical illness. No statistically significant difference was found between ictal EEG patterns and underlying neurological versus medical etiologies (p=0.27) or in-hospital mortality (p=0.5).
Significance
Spatiotemporal evolution of epileptiform discharges at a lower frequency was the most commonly recorded ictal EEG pattern in our cohort. Further prospective studies with a larger sample size of patients with NCS may provide valuable clinical data that could be used to evaluate the etiologic correlate of the various ictal EEG patterns and their effect on outcome.