Hépato-Gastro & Oncologie Digestive
MENUNutrition in acute pancreatitis Volume 24, issue 10, Décembre 2017
- Key words: acute pancreatitis, malnutrition, enteral nutrition, parenteral nutrition
- DOI : 10.1684/hpg.2017.1546
- Page(s) : 1030-9
- Published in: 2017
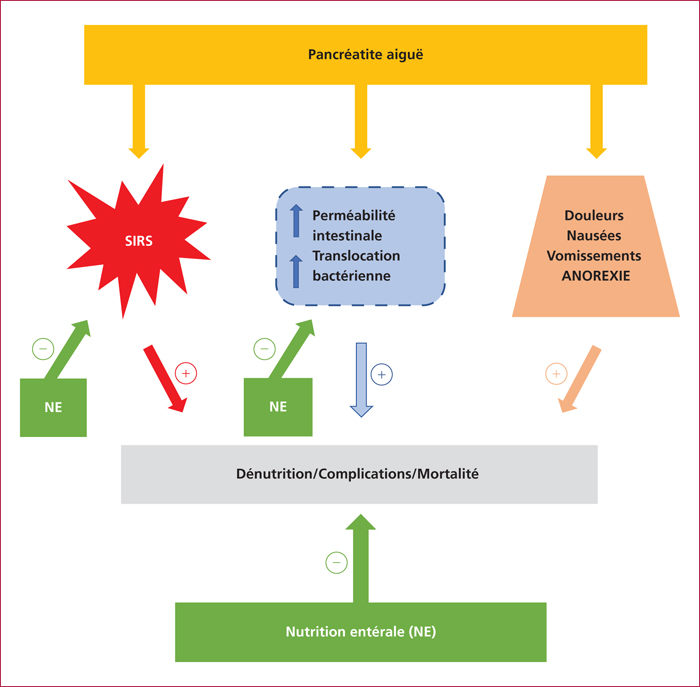
In acute pancreatitis (AP), numerous data have demonstrated that several factors contribute together to have a negative impact on nutritional status. This is the case of acute inflammation with the occurrence of the Systemic Inflammatory Response Syndrome which can lead to multiple organ failure (MOF), pain, nausea and vomiting inducing anorexia and a decrease in nutritional intake, and inflammation-induced alterations of the gut barrier leading to bacterial translocation and its deleterious consequences. The resulting hyper-catabolic state as well as the other metabolic disturbances observed in AP increase its morbidity and mortality.
Therefore, and despite some clinicians still believe that patients with AP, at least in the early phase of pancreatic injury, may benefit from fasting, it is important to know that early nutritional support does not harm to the patients, but by contrast, has been recognized as an important tool of AP treatment.
Especially in severe AP, enteral nutrition (EN) is recommended by international guidelines to be started within 48 hours from admission. This EN could be administered through a nasogastric feeding tube and can use standard polymeric EN formulas. The energy and nutritional substrate requirements have been clearly established. Parenteral nutrition (PN) should be avoided (and only used if the enteral route is not feasible) as PN increases the rate of infectious complications and has been reported in several studies to increase the risk of MOF and of overall mortality.
The aim of this review is to highlight the role of early nutritional support in patients presenting AP.