Epileptic Disorders
MENUKnowledge gaps for functional outcomes after multilobar resective and disconnective pediatric epilepsy surgery: Conference Proceedings of the Patient-Centered Stakeholder Meeting 2019 Volume 24, issue 1, February 2022
The prevalence of pediatric epilepsy is 3.2-5.5/1,000 children [1]. In a subset of patients who prove to be medication-resistant (i.e. not seizure-free after trialing two or more antiseizure medications) [2], epilepsy surgery may be the most effective way to achieve seizure freedom in appropriately selected children [3]. Infants and young children with surgically remediable epilepsy often require multilobar or hemispheric surgeries, which can include resection of large areas of cortex and/or disruption of fiber tracts [4]. Though such large resections are often successful at achieving seizure freedom, disruption of functional cortex may lead to permanent neurocognitive and motor deficits [5, 6]. A major limitation of the existing literature is that no studies comprehensively address the cognitive, medical, behavioral, orthopedic, and sensory consequences across the lifespan following large epilepsy surgeries in childhood. The limited evidence available in this diverse group of epilepsy surgery patients leads to anxiety and uncertainty for parents and clinicians who navigate the chronic phase of recovery without so much as a basic roadmap.
Historically, the most commonly studied metric for epilepsy surgery outcomes has been short-term seizure freedom, with minimal attention to long-term outcomes. While early surgery is critical to prevent developmental regression in infants with severe epileptic encephalopathies, the 2003 meeting of the Pediatric Epilepsy Surgery Subcommission of the International League Against Epilepsy (ILAE) argued for further studies of medication-resistant epilepsy in childhood to determine whether the developmental benefits of early surgery for epilepsy exist for the entire pre-adolescent population [7]. Subsequent publications have called for long-term follow up studies to understand the impact of epilepsy surgery at different developmental periods, however, despite this call for functional outcome research, the body of publications is limited in the realms of motor function, cognition, behavior, and quality of life. This lack of empirical information about long-term outcomes may contribute to parental and professional reluctance to consider surgery and delay referral for presurgical evaluation [8, 9]. Such delays lengthen the duration of epilepsy prior to surgery, a factor that is correlated with poorer postsurgical adaptive function [10]. Thus, characterizing the long-term functional outcomes is of paramount importance for guiding presurgical evaluations and minimizing duration of presurgical epilepsy, while informing methods of postsurgical intervention to achieve superior outcomes beyond seizure freedom.
In the U.S., the utilization of pediatric epilepsy surgery to stop medication-resistant seizures has nearly doubled over the previous decade although it continues to be underutilized for children with medication-resistant epilepsy [11]. Despite this increase and the ILAE's call for clinical studies to assess outcomes after epilepsy surgery, there is much that remains unknown about the long-term functional outcomes of epilepsy surgery, especially with regard to large multilobar or hemispheric epilepsy surgery. To further inform understanding, a meeting was convened by The Brain Recovery Project: Childhood Epilepsy Surgery Foundation (BRP), a patient advocacy organization that funds research and provides information, advocacy, and support services to parents and caregivers of children who require surgical treatment for refractory epilepsy. The purpose of the meeting was to align on the current state of research gaps that exist around long-term functional impacts of large resective and/or disconnective pediatric epilepsy surgeries. Prior to the meeting, convening group members developed a set of preliminary patient-centered outcomes research (PCOR) goals and objectives [12], driven in large part by the needs and gaps identified by parents, caregivers, and adult patients.
The objectives of the meeting were: (1) to establish a cross-sector patient-centered outcome research collaboration committed to advancing research on the long-term functional impacts of resective and disconnective pediatric epilepsy surgery; and (2) to develop a patient-centered research agenda which identifies the top three to five research priorities and objectives related to long-term functional impacts of resective and disconnective pediatric epilepsy surgery.
As a summary of proceedings, the major content of the presentations given at the conference from a group of experts within the field is reported here. This report is therefore intended to disseminate the current state of research in functional outcomes from a convergent group with expertise and does not represent a systematic or comprehensive review of the literature.
Summit organization
Stakeholder engagement
To ensure the meeting maintained a patient-centered approach, we developed a PCOR planning committee comprised of parents/caregivers, adult patients, researchers, and clinicians. Participants were selected by the Project Lead as follows: patient stakeholders were identified based on their prior engagement with BRP, advocacy group alignment, as well as diversity of backgrounds; clinicians and researchers with content expertise were similarly identified, many of whom were members of BRP's Scientific Advisory Board. The diverse group of stakeholders were engaged to identify the most relevant and urgent issues for parents caring for children after epilepsy surgery. In addition to the PCOR planning committee, the BRP's Community Advisory Council, comprised of parents/caregivers and adults who had surgery in childhood, was invited to set-forth future research topics and issues to be discussed at the planned summit.
The “Functional Impacts of Large Resective or Disconnective Pediatric Epilepsy Surgery: Identifying Gaps and Setting PCOR Priorities” meeting (Stakeholder Meeting) was convened on July 18, 2019, to identify gaps in knowledge and inform various patient-centered research initiatives. The PCOR planning committee invited individuals representing three stakeholder groups: patients (identified as parents, caregivers, and adults who had surgery in childhood, as well as patient education and advocacy groups), clinicians (including professional societies), and researchers. The 43 participants represented a cross-section of patients, family members, advocates, practicing clinicians, professional societies, patient advocacy organizations, and researchers (see supplementary material).
Prior to the PCOR Stakeholder Meeting, pre-recorded webinars were hosted for stakeholders to educate them on the processes and value of patient-centered research and to clarify their specific role in this project. The webinars also provided an overview of the meeting goals, agenda, and future course.
The Stakeholder Meeting was an all-day, in-person meeting organized by pre-identified functional outcome areas: motor and orthopedic; cognitive; educational; behavior and sensory; speech and language; and medical. A patient/parent stakeholder perspective was given for every functional outcome area, followed by presentations from clinicians and researchers that synthesized the extant research in that area. In an effort to ensure discussions were accessible to the patient stakeholders in this group, researchers and clinicians were asked to refrain from using medical jargon and citations in their talks (sharing them later in print form instead). Following presentations for each functional outcome area, small groups comprised equally of clinicians, researchers, parents/caregivers and adult patients met to discuss specific gaps in evidence and critical research needs for each functional outcome area. These groups allowed patients and parents to share their personal experiences while engaging alongside a variety of clinicians and researchers.
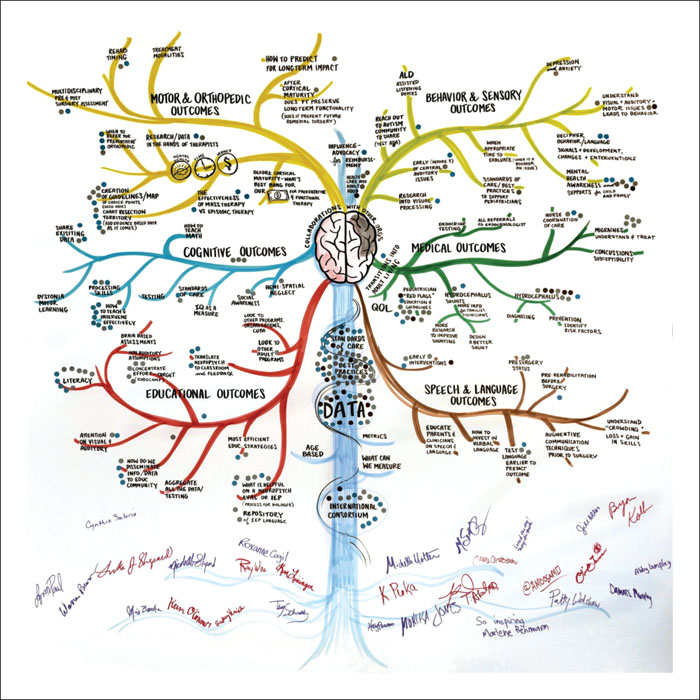
A professional meeting facilitator aided the discussion, while the main points and key takeaways from each presentation were captured in real-time by a graphic recorder who created hand-drawn visual notes on large foam boards. The graphic recorder also created a large, hand-drawn idea map depicted as a modified tree, with each functional outcome area represented by a branch (figure 1). Following small group discussions about each functional outcome area, all participants convened by the tree drawing for a facilitated discussion, and the whole group of stakeholders identified future research goals which were recorded on the idea map. At the end of the day, stakeholders voted individually on research topics which should be given highest priority, by placing 1 to 10 round stickers beside any topic on the idea map. The votes (stickers) were tallied and the results defined the research priorities. All topic ideas were captured in the graphic recording for further review.
Finally, a lay summary of the meeting and video-recorded clinician sessions with the parent/caregiver and adult patient community was shared online [13] and via social media channels. To date, the web page summarizing the meeting and video-recorded sessions has been viewed over 900 times.
Conference presentations
Brain plasticity
The summit commenced with Dr. Bryan Kolb giving a keynote address on brain plasticity, a fundamental principle that likely contributes to the functional outcomes following epilepsy surgery, particularly in children. Plasticity is age-specific, with the human brain increasing in number of neurons and connections until approximately ages 2-5 years, depending on the region of the brain [14]. Synaptic pruning ensues until at least age 30 years, with a peak during puberty [15]. Plasticity is an adaptive process influenced by epigenetics; the genetic changes associated with experience and behavior. In the instance of epilepsy, plasticity can also be a maladaptive process leading to progressive brain deterioration. Following surgical resection, however, altered processing can lead to altered behavior, the extent of which depends on the size of the injury. Suggested treatments to optimize functional outcomes from a neuroplasticity perspective include, in combination or adjunctive to pharmacologic therapy: tactile stimulation, constraint-induced therapy, treadmill training, virtual environments, robotic devices, behavioral shaping, and task-oriented physical therapy [16].
Clinician and researcher insight
In a panel-wide discussion, six different expert clinicians and scientists provided their perspectives on postoperative functional outcomes of pediatric epilepsy and the impact of brain plasticity. The consensus was that current understanding of functional outcomes is limited, primarily a result of insufficient research or research limited by short-term follow-up.
However, there were a few general principles consistent throughout. For example, it is often stated that early age at surgery is associated with improved outcomes owing to maximal potential of brain plasticity; on the other hand, this is not always the rule. Functional outcomes can also be influenced by the extent of tissue that must be resected or disconnected. Whereas epilepsy surgery is a disease-modifying intervention, treatment with antiseizure medications is not. It is therefore difficult to compare the impact of epilepsy surgery in medication-resistant children to their age-matched counterparts that continue medication therapy. Further, epilepsy surgery is personalized medicine; the potential functional effects of surgery are specific to the child, not the surgery performed. If significant pre-existing developmental problems exist, it is unlikely that the child will recover all of the lost or unmet developmental milestones the parent desires. Surgery, nevertheless, has the advantage of potentially preserving function that has not yet been lost to the epilepsy.
A summary of the best available evidence presented by 12 respective experts has been compiled (tables 1-3). The sections below provide a brief content overview for each functional domain synthesized from the experts’ individual presentations.
Motor and orthopedic outcomes
There are no studies on long-term functional orthopedic outcomes after resective or disconnective pediatric epilepsy surgery. The existing studies on motor outcomes after hemispherectomy (e.g., foot, knee, gait, muscle, locomotion, motor) suggest that hemiparesis is worse in half of children after surgery, arms are more affected than legs, and hand/wrist function is more affected than elbow/shoulder, sometimes never returning to the same degree of preoperative function [17]. Children who were ambulatory preoperatively remain ambulatory after surgery [10], and 25% of children who were not ambulating preoperatively gained ambulation [18]. While the timeline for ambulatory function is unknown, general motor skills improve over time up to at least two years after surgery [19, 20]. Whether further motor progression is possible is limited by lack of long-term follow-up. Factors associated with good motor outcomes include shorter duration of seizures before surgery, higher level of overall development, and younger age at the time of surgery [10, 18, 21]. The effect of etiology on outcome varies, but acquired etiologies (e.g., perinatal infarction) may have better outcomes than congenital causes (e.g., hemimegalencephaly) [19]. Because few studies exist after 2013, particularly with large sample populations, no clear consensus can be drawn from existing data to guide counseling on motor and orthopedic outcome in this cohort (table 1).
Cognition and education outcomes
For children undergoing hemispherectomy, the neuropsychological status is unchanged in 61%, improved in 29% (by 15 IQ points), and declined in 10% [22]. No patients with bilateral disease show improvement [23]. In terms of academic achievement, 65% of patients can read, 61% can write, and 3% have arithmetic skills beyond counting [24]. Patients with a remaining right hemisphere are able to achieve word reading outcomes that are inferior to those with a remaining left hemisphere, but comparable to peers with developmental dyslexia [25]. In the long-term follow up of children undergoing hemispherectomy, intelligence ranged from severely impaired to low-average [24]. Baseline data on these skills has not been systematically collected prior to surgery; it is not yet possible to ascertain the impact of surgery per se. Change in educational outcomes can be difficult to evaluate given that baseline assessments may not be possible as a result of the child's young age at the time of surgery. Pediatric epilepsy encompasses a wide age range that requires different tests for different ages, posing another challenge to longitudinal monitoring.
Because memory is an important indicator of quality of life and key to learning, it is important to understand the effect surgery has on memory. Given the role of the hippocampus in memory formation, most studies exist on children undergoing temporal lobe resections and hippocampectomy. At the study level, 11/18 studies suggest stability in memory after temporal lobe resection, with 75% unchanged, 9-14% improved, and 10-14% declined; whereas at the individual level, 57% remain stable, 17% improve, and 25% decline after surgery [26]. Following left temporal resection, one cohort of children with lateral resection only demonstrated near return to baseline in verbal memory, while another group with mesial (i.e., involving hippocampus) and lateral resection showed significant decline in verbal memory one year after surgery [27]. In the long-term, memory does not significantly differ between children with epilepsy who undergo surgery compared with those who do not [28]. Children with lower baseline scores [28] and unilateral non-dominant hemisphere lesions preoperatively [29] tend to have the greatest improvement postoperatively.
To gain insights about mechanisms - and limits - of compensation following childhood hemispherectomy, one research group conducted in-depth cognitive assessment of adults with limited global cognitive impairment post-surgery. Preliminary results suggest that ‘good’ long-term cognitive and adaptive outcomes are associated with relative strength in post-operative verbal skills, regardless of which hemisphere was removed. There is also evidence that adults who have undergone hemispherectomy as children underestimate their difficulty with everyday adaptive behavior.
Much more research is needed to understand how children learn and recover cognitive abilities and education-related skills post-surgery. Characterizing cognitive and academic abilities longitudinally from presurgical evaluation to adulthood in a large sample that is representative across multiple critical factors (e.g. age at seizure onset, epilepsy etiology, age at surgery, resection area) is an ambitious goal, but it may be possible through the coordinated effort of multiple researchers. First steps toward this goal involve establishing a research consortium, implementing a common standardized test battery across sites, and building a centralized data-sharing system. Through this effort, we can identify factors that predict functional outcome and cognitive skills to target for optimizing recovery (table 2).
Behavior and sensory outcomes
There are very few data with sufficient specificity and generalizability to inform parents and caregivers on how resective and disconnective epilepsy surgery will impact their child's behavior and mental health— and how to intervene. Children with epilepsy, including surgical candidates, have higher rates of mood and behavioral concerns [30, 31]. The prevalence may be higher in children with developmental compared to acquired etiologies. Favorable behavioral outcomes are associated with seizure freedom [32], whereas unfavorable outcomes correlate with younger age at seizure onset and temporal or frontal lobe involvement [27]. Children's quality of life is more strongly associated with their mood than with seizure control [33].
In general, there is short-term stabilization or improvement seen following surgery [32]. Conversely, some children undergoing epilepsy surgery with no change at three months have seen significant improvement at two years [34]. One study showed that, after hemispherectomy, 27% of children have significant behavioral symptoms [35], however, 92% experience improvement from baseline in at least one domain [36] and significant improvement has been seen in 57% of children studied [37]. Children undergoing lobar resections tend to have improvements in externalizing behavior, aggression, and social skills [38], but about half have a mental health diagnosis postoperatively [30].
Because the auditory systems fuel speech and learning, including literacy acquisition, it is important to understand the impact of pediatric epilepsy surgery on the auditory systems. Impairment of the auditory systems following resective and disconnective surgery often goes undetected because most children will pass an audiogram. A normal audiogram does not equal normal hearing and will not reveal a central auditory processing issue. In fact, hemispherectomy patients have demonstrated significant deficits in contralateral dichotic hearing, approaching frank contralateral auditory neglect [39]. They also have had poor sound localization, 30 degrees worse than controls, as well as discrimination of sound in noisy backgrounds. More research is needed to identify symptoms related to central auditory deficits in post-multilobar resection/disconnection patients which is essential in providing them with effective interventions including auditory training and assistive listening devices.
Given that the primary visual cortex is located posteriorly, resection or disconnection of this region (e.g., hemispherectomy) invariably results in a contralateral hemianopia. This visual deficit is typically persistent and stable, with no obvious reorganization on the healthy side. However, it has been shown that visual processing and intellectual performance are not necessarily impaired by hemianopia [40]. In contrast to posterior resections, patients with focal anterior resections (e.g., anterior temporal lobectomy) may have fully intact visual fields without deficit [41]. Further, preliminary data have suggested that the visual tracts distal to anterior resections do not degenerate, as can be seen in other white matter tracts. More research needs to be done with a larger sample size to understand the impact of surgery on vision and visual processing (table 1).
Medical outcomes
The incidence and prevalence of endocrine issues after large resections is not well reported and poorly defined; very little published information exists. Similar endocrine dysfunction to that seen in hypothalamic hamartoma [5] has also been reported anecdotally in children undergoing larger resections for epilepsy, namely precocious puberty. Children undergoing large epilepsy surgeries are also at risk of other hypothalamic-pituitary dysfunction, including diabetes insipidus, adrenal insufficiency, growth hormone deficiency, thyroid deficiency, and hypothalamic obesity. Because the presence of comorbid endocrine dysfunction can increase morbidity and reduce quality of life [42], more careful baseline and postoperative evaluation is recommended. Endocrine dysfunction of the pituitary gland is most likely secondary to injury of the hypothalamus. This can occur by an aggressive disconnection or an expanding third ventricle in the case of hydrocephalus. Studying children with brain tumors and hydrocephalus may provide insight.
Hydrocephalus, an imbalance between cerebrospinal fluid (CSF) production and absorption, is the most devastating of the potential complications and affects all other domains. There is no cure for hydrocephalus; the only effective interventions are surgical. Research on postoperative hydrocephalus is severely limited. Only two studies exist [43, 44] and only one is multi-center. Hydrocephalus is predominantly a complication of hemispheric procedures and has been found to occur in 23-30% of patients post-hemispherectomy, though the prevalence may be lower among contemporary cohorts. The most commonly presenting sign is failure to wean the cerebrospinal fluid (CSF) drain after surgery. Major risk factors associated with shunt requirement include anatomic hemispherectomy and repeat surgery, and underlying etiology may also influence the risk [43]. Intraoperative factors that may reduce the risk, by expert opinion, include disconnecting rather than resecting the hemisphere, decreasing blood loss at surgery, decreasing the amount of blood in the ventricles, and aggressive postoperative CSF drainage. Large prospective multicenter studies are needed to identify strategies to lower the prevalence of postoperative hydrocephalus and optimize management in those who develop this complication (table 3).
Speech and language outcomes
One of the most important concerns parents/caregivers have when faced with the option of large pediatric epilepsy surgeries is whether or not surgery will impact a child's ability to speak. Though it is commonly believed that children who undergo surgery outside of early childhood may be greatly impacted in the areas of speech and language, there are studies that demonstrate greater language impact from surgery in early childhood [35] and other studies that demonstrate some recovery with later resection [45, 46]. Contrary to popular opinion, there is no clear age identified for which interference with hemisphere structure or connectivity will have the greatest impact on language. Because language lateralization rapidly increases with age [47], however, earlier surgery provides a greater chance for compensation by the healthy side when primary language areas are involved in resection. Other factors that predict better language outcomes include seizure control after surgery and developmental level before illness [21, 35].
Rather than surgical timing, language outcomes are more strongly associated with etiology [48]. Patients with hemimegalencephaly and severe preoperative deficits tend to have poor language outcomes, whereas those with perinatal stroke have the best language recovery [21, 49]. Primary areas responsible for basic comprehension tend to recover best, areas responsible for expressive speech may recover at least some function postoperatively, while regions responsible for higher order language functions (e.g. reading) may have limited recovery [35, 45]. There are limitations to understanding language outcomes after surgery, however, as few current studies have sufficient sample sizes. Though underexamined, language organization prior to surgery is an essential factor in determining recovery and outcome (table 2).
Consensus priorities
Among the functional outcome areas, the group identified research gaps and priorities (table 4). Through active discussion between stakeholders, the following were identified as the three most important research priorities:
- •Research around postoperative hydrocephalus;
- •Research around post-surgical mental health issues;
- •Research around literacy and educational interventions.
Several subject matter experts agreed to establish a patient-centered research consortium to inspire and initiate studies around the three research priorities. Additionally, plans were made to develop an article proposing best practice guidelines for symptom surveillance and treatment based on existing knowledge, which would be shared at professional meetings by the consortium members.
Post-summit evaluations
Of the stakeholder participants who completed post-evaluation surveys (86%, n = 37), all strongly agreed or agreed that they had a better understanding of the current landscape of research, the gaps that exist, and a better understanding of their role and the critical importance of driving patient-centered outcome research.
Discussion
A group of committed stakeholders gathered to collectively consider the current state of research around functional outcomes after large pediatric epilepsy surgeries, to identify research gaps, and to set patient-centered research priorities. The recommendations from this conference proceed from consensus reached by the participants. This is the first time that research on functional outcomes after resective and disconnective pediatric epilepsy surgery has been codified and shared, alongside parents/caregivers and adult patients who were invited to share their real-life experiences to illuminate and give life to the research.
For adult patient and caregiver stakeholders, one immediate outcome was a better understanding of the extant research, and the best practices in post-surgical care. For example, parents and caregivers were provided information about the types of endocrine challenges that are most likely to impact children who undergo resective or disconnective surgeries, and they can now take action to establish care with an endocrinologist to establish baseline measures, proactively monitored for potential complications. Adult patient and caregiver stakeholders also gained a deeper understanding of the variables and predictors that could impact a child's long-term functional outcome, and how those variables can impact research findings.
As a result of the meeting, clinicians recognized the critical role they need to play in directing the management of long-term follow-up care. Another outcome for clinicians and researchers was the understanding that more baseline functional data are needed to accurately assess the impact of the intervention. Compared with standalone postoperative data, this will have much greater implication for parents and physicians making decisions about surgery and postoperative management. Importantly, researchers identified patient-important outcomes to pursue in collaboration with this community of advocates.
One of the most powerful insights gained by participants at this meeting is the future for many children and their families which is directly dependent on the collaborative effort and shared wisdom of stakeholders from all groups (parents/caregivers, adult patients, researchers and clinicians). Clinicians and researchers began discussing the need for a research consortium to facilitate sharing of research and medical data across fields and across sites – an approach that is gaining traction for studying rare diseases and will be very powerful for studying rare procedures. Sharing medical data is uniquely challenging, particularly for such unique and easily-identifiable patients, but it is a hurdle that must be overcome.
Conclusion
The lack of literature available to clinicians and families on functional outcomes of pediatric epilepsy surgery leaves all stakeholders underinformed with regard to counseling and expectations. Improved understanding of these areas may allow parents and clinicians to identify and address functional deficits proactively in order to optimize outcomes across domains. As a result of the meeting, the top research initiatives were identified from close collaboration between clinicians, researchers, and patients/caregivers. This joint initiative promotes continued funding and research in this field, ensures that the progress heads in a direction that aligns with actual patient and family experience, and aids improved counseling for postoperative expectations and postoperative management for children undergoing epilepsy surgery.
Supplementary material
Supplementary data accompanying the manuscript are available at www.epilepticdisorders.com.
Funding
This program was partially funded through a Patient Centered Outcomes Research Institute® (PCORI®) Eugene Washington PCORI Engagement Award (EAIN - 00024)). The views, statements, and opinions presented in this publication are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors or Methodology Committee. Additional funding was received from the American Epilepsy Society and DIXI Medical.
Disclosures
None of the authors have any conflicts of interest to declare.