Epileptic Disorders
MENUUnilateral catalepsy in non-convulsive status epilepticus Volume 23, numéro 5, October 2021
Catalepsy is a condition characterized by inactivity, decreased responsiveness to external stimuli, and a tendency to maintain fixed postures imposed by the examiner, however bizarre and uncomfortable, for prolonged periods. It often represents a prominent sign of catatonia, a complex neuropsychiatric syndrome characterized –among others – by mutism, waxy flexibility, stereotypies and mannerisms, excitement, automatic obedience and echopraxia/echolalia. However, catalepsy has also been described in association with neurodegenerative disorders as well as focal brain injuries, such as ischemic or haemorrhagic strokes, involving either cortical (mainly frontal, temporo-limbic and parietal) or subcortical (i.e. basal ganglia, thalamus, brainstem) structures [1-3].
Here, we present the first case of a patient with focal non-convulsive status epilepticus, manifesting as unilateral catalepsy.
Case study
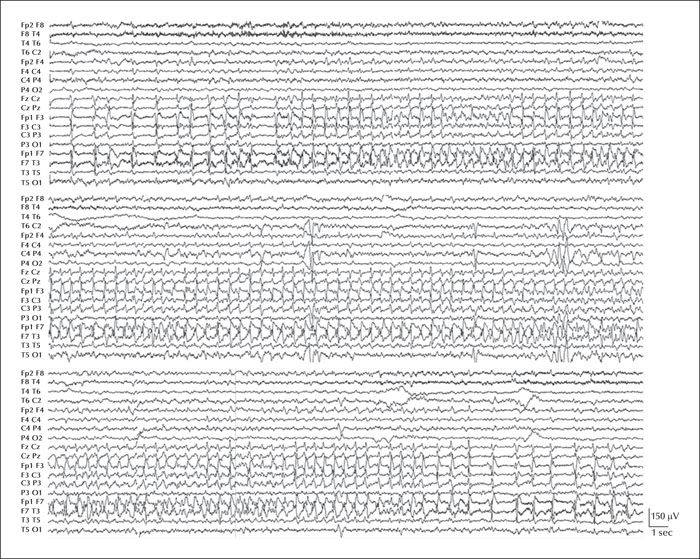
An 81-year-old, right-handed man was admitted to our hospital due to a brief episode of right-gaze deviation with concomitant impairment of awareness. He had a history of left middle cerebral artery stroke, resulting in right hemiplegia and slight non-fluent aphasia. Three months before hospitalization, he had a large left frontal meningioma that was surgically resected. Upon admission to our ward, neurological examination revealed global aphasia, verbal perseveration and catalepsy of the left limbs, particularly affecting the arm (video sequence 1). An EEG examination documented sub-continuous spike/polyspike-and-slow-wave activity, intermingled with brief periods of EEG flattening, located over the left fronto-central and temporal regions (figure 1), consistent with focal non-convulsive status epilepticus (NCSE). During the ongoing NCSE, the EEG recording also showed brief focal seizures arising from the left frontal region (figure 2), clinically associated with transient impairment of awareness, gaze and head deviation towards the right, and inconstant bilateral rhythmic blinking.
The brain MRI scan revealed extensive gliosis in the left frontal lobe, secondary to the previous neurosurgical procedure; moreover, it documented an increased diffusion-weighted signal with a corresponding drop in ADC values involving the left frontal cortex (cortical ribboning), compatible with cytotoxic oedema (supplementary figure 1). This finding was interpreted as the correlate of intense metabolic and haemodynamic changes, possibly related to NCSE. Lacosamide (loading dose of 400 mg) was administered intravenously, followed by daily oral maintenance therapy. Two days later, the patient showed a marked clinical improvement with catalepsy remission, matched by EEG normalization.
Discussion
We report a case of unilateral catalepsy related to EEG-documented NCSE in an elderly subject. From a semiological point of view, our patient presented a tendency to maintain bizarre postures imposed by the examiner, for several minutes. We interpreted these manifestations as isolated catalepsy, which is per se a rather uncommon phenomenon, since catalepsy is generally observed in the context of a more complex catatonic syndrome. Indeed, it represents the most specific sign of catatonia, although its sensitivity is limited (in fact, catatonia occurs in only 27% of cases) [4]. Our case appears even more peculiar considering that catalepsy was observed in concomitance with NCSE, affecting the fronto-central and temporal areas, and subsided when NCSE abated. Such temporal correlation, along with the absence of other more common etiological factors (e.g. anti-dopaminergic drugs, prior psychiatric diseases), clearly points to the epileptic origin of our patient's catalepsy. This hypothesis was also supported by the neuroimaging study, showing frontal cortical ribboning, compatible with “peri-ictal” metabolic changes [5]. To our knowledge, ictal catalepsy has not previously been described, whereas catatonia has been rarely correlated with epilepsy [6]. In particular, three catatonic patients with NCSE (either generalized or focal) of unknown aetiology were reported by Lim and colleagues [7], whereas other authors occasionally described catatonia during absence status epilepticus in the context of both idiopathic generalized epilepsy [8] and benzodiazepine withdrawal [9]. Interestingly, in most of these reports, patients had a concomitant/previous psychiatric illness, contrary to our patient.
Although the pathophysiological mechanisms underlying catalepsy have not been specifically investigated, it is likely that frontal lobe dysfunction plays a key role in our case. Indeed, the ictal EEG pattern appeared prominent on the frontal derivations, and concurrent verbal perseveration, suggestive for a frontal dysfunction, was also observed. Therefore, it could be hypothesized that in our patient, the enduring epileptic activity resulted in the disruption of a complex cortico-subcortical network, involving, in particular, the basal ganglia and the frontal cortices, possibly favoured by the pre-existent left hemisphere lesions. This hypothesis is in accordance with previous studies [10-12], suggesting that the impairment of an extensive dopaminergic network could result in catalepsy [2, 13].
Notably, our patient's catalepsy was unilateral, and only affected his left limbs. Such a finding is rather unusual, since bilateral cases, either symmetrical or asymmetrical, have been more commonly reported [1, 3]. Moreover, our patient's cataleptic limbs were ipsilateral to the EEG-documented NCSE, which might seem paradoxical. In fact, this is in line with five post-stroke catalepsy cases described by Saposnik and colleagues [14], and might be justified by the pre-existing right hemiplegia, which prevented us from properly evaluating the contralateral limbs.
Finally, our report is of interest as, once again, the clinical overlap between epilepsy and movement disorders (MDs) is demonstrated, making differential diagnosis challenging for physicians in routine practice. Indeed, both conditions can manifest with abnormal movements, such as myoclonus and dystonia. Moreover, some genetic syndromes (for instance, GLUT1 deficiency and paroxysmal kinesigenic dyskinesia) are characterized by the co-occurrence of seizures and paroxysmal MDs, suggesting a common pathophysiological background. Therefore, a systematic diagnostic approach is always recommended in patients presenting with abnormal motor phenomena, including rare hypokinetic phenomena such as catatonia and catalepsy.
In conclusion, to the best of our knowledge, this is the first report of isolated unilateral catalepsy as the sole manifestation of focal NCSE, and suggests that frontal lobe dysfunction could play a crucial role in the genesis of catalepsy.
Supplementary material
Supplementary figure accompanying the manuscript is available at www.epilepticdisorders.com.
Disclosures
The authors report no disclosures relevant to the manuscript.