Journal de Pharmacie Clinique
MENUImpact of medication reconciliation on prescription errors at discharge from an internal medicine ward Volume 37, issue 4, Décembre 2018
- Key words: medication reconciliation, patient discharge, internal medicine, clinical impact
- DOI : 10.1684/jpc.2018.0402
- Page(s) : 215-24
- Published in: 2018
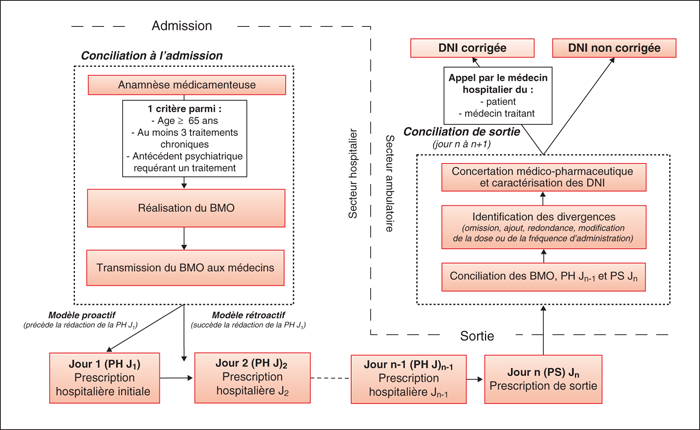
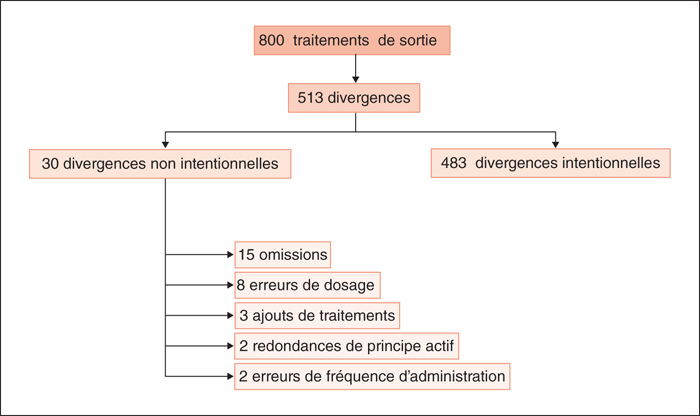
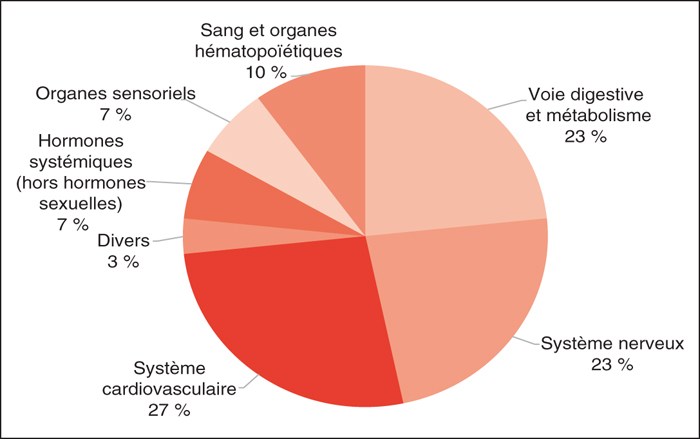
The hospital-community transition places patients at an increased risk of having unintended medication discrepancies at the time of discharge. By comparing usual patient's medication list with hospital and discharge medication lists, medication reconciliation prevents this risk. The study aims to determine unintended medication discrepancies prevalence and to assess medication reconciliation impact at the time of discharge. During 6 months, medication reconciliation was performed by a clinical pharmacist within the 24 hours following the discharge from an internal medicine ward. Patients were included if they were discharging to home and had a medication reconciliation at admission. For each unintended medication discrepancies, the therapeutic ranking value (according to the French Health Authorities ranking), the potential clinical impacts and the number of prescriptions corrected after the intervention of the clinical pharmacist were assessed. One hundred patients were enrolled consecutively. Of the 800 prescribed medication at the discharge, the prevalence of the unintended medication discrepancies was 3.75% (n=30) and involved 24 patients. Discrepancies concerned 7 therapeutic classes, 24 had an important or a major therapeutic ranking value and 14 had a potential clinical impact. Twelve unintentional medication discrepancies were corrected after discharge. Both medication reconciliation at discharge and at admission secure medication prescription while consolidating the collaborative practices between medical and pharmaceutical staffs. A proactive approach anticipating medication prescription at discharge could result in a better prevention of unintentional medication discrepancies.